The War on Germs
Kill Them Before They Kill You!
Since the Golden Age of microbiology, when the connections between bacteria and disease were first revealed and Semmelweis started washing his hands, Pasteur postulated the Germ Theory, and Lister promoted aseptic surgery, we have become obsessed with destroying microbes. As a result, companies that make products to “kill” microbes—whether to have a cleaner home or to cure bacterial infections—make a killing off of us as we rush to acknowledge the effectiveness of marketing campaigns that tell tales about “evil germs” that must be “killed on contact.”
In reality, promoting the need for humans to live in a germ-free world is misguided and in some cases perhaps even dangerous. The overwhelmingly beneficial nature of our microbiome and its metagenome is now well established. Overuse of personal and environmental hygiene products and antibiotics has resulted in the logical evolution of bacterial resistance to them. As Friedrich Nietzsche (and Kelly Clarkson) famously said, “That which does not kill us makes us stronger.” This certainly bears true for bacteria. Some bacterial pathogens are now resistant to every type of antibiotic available. Bacteria acquire antibiotic resistance through mutation and natural selection, and once such traits are acquired, they are shared with other bacteria by horizontal gene transfer. Infectious diseases once thought defeated, such as tuberculosis and pneumonia, are again climbing the ranks on the mortality charts.
We are destined to live in a microbial world. Prudent use of antimicrobial products is a necessity, particularly in healthcare settings where sanitation practices and infection control are essential. Available are a large number of chemical and physical agents that are used for sterilization (killing or removal of all microorganisms) and disinfection (reducing the numbers of microorganisms) that are widely used to control microbial growth. But how do you know if they work?
Chemicals used to kill microbes damage cell components through chemical reactions with proteins, membranes, or other parts of bacterial cells. Heat, cold, and radiation are physical agents that inhibit or inactivate microbes in food, on surfaces, and even in the air. Bacteria exhibit a wide range of susceptibilities to these agents. For example, Gram-positive bacteria can withstand higher heat and more radiation, while Gram-negative bacteria tend to be more resistant to chemical destruction. Microbial susceptibility to antibiotics varies widely.
Selective removal of pathogenic microbes that spares or minimally damages body cells has long been the goal of medicine. Paul Ehrlich was searching for just such a “magic bullet” when he found the first real antibiotic, the arsenic-based compound Salvarsan for treatment of syphilis, in 1910. Now we realize there can be no magic bullet, because to one extent or another, antibiotics wreak havoc on our bacterial symbionts as much as the targeted pathogen, and those bacteria are as much a part of us as are our own cells.
Some antibiotics are effective against a narrow spectrum (or range) of bacteria, such as the antibiotic isoniazid which is only used to treat infections caused by mycobacteria. Broad spectrum antibiotics work against a wide range of taxonomic groups. In medicine, the preferred approach is to minimize damage to the microbiota by applying a narrow spectrum drug first, which also decreases the risk of promoting antibiotic resistance. Testing pathogen susceptibility to several types of antibiotics while the bacteria grow in culture is the preferred way to evaluate which to use for chemotherapy of the infection.
Several culture-based methods have been developed for this purpose. One of the most widely used methods is the disk diffusion test, used to assess the antimicrobial activity of chemical agents. The Kirby-Bauer assay, used in clinical laboratories to evaluate which antibiotics are effective against a bacterial pathogen, is a standardized form of disk diffusion test that follows a strict protocol (e.g. type of medium used, temperature and time of incubation) so the results can be compared across labs.
Kirby-Bauer Disk Diffusion Assay for Antimicrobial Susceptibility
After the widespread use of antibiotics began in the 1950s, one of the first observations made was that they didn’t work for every infection. Thus test methods to evaluate susceptibility were developed. The earliest versions were based on broth dilution methods, which although very useful for determining the level of susceptibility to various concentrations of the drug, were time and labor-intensive to perform. And so the disk diffusion method was developed.
The disk diffusion method was widely adopted as the standard method for antimicrobial testing by clinical labs in the US by the end of the 1950s. Basic procedures were modified to suit the locally available resources and expertise, and interpretation of results began to vary widely by lab.
Kirby and colleagues (including Bauer) were the first to propose that standardization of the method was necessary for uniformity across labs, and developed the method that still bears their names: the Kirby-Bauer assay.
Of major importance to the success of this method is to inoculate test plates with approximately the same number of bacterial cells each time the test is performed. A relatively simple way to achieve a uniform number of cells in the inoculum is to first prepare suspensions of bacterial cells in sterile saline, which may then be compared, either using an instrument such as a spectrophotometer or by direct visual comparison, to an optical standard matching a known concentration of bacteria. Typically a 0.5 McFarland standard is used. This is equivalent to a bacterial suspension containing between 1 x 108 and 2 x 108 CFU/ml of E. coli.
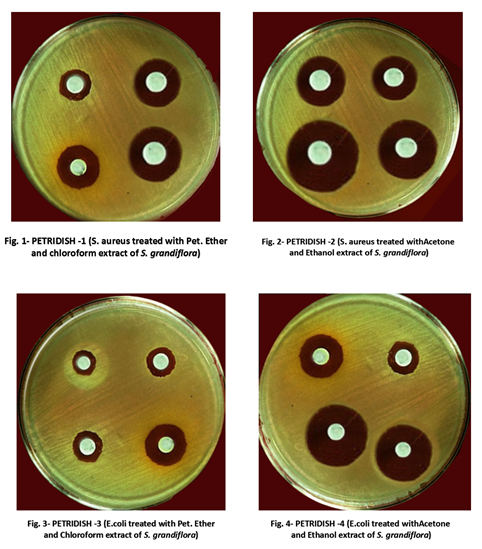
Standardized cell suspensions are then inoculated onto the surface of a specific type of medium using a sterile swab. The plates are inoculated to completely cover the surface of the medium with bacterial cells, which then grow into a lush “lawn” of colonies. Once the lawn is “seeded,” a filter paper disk saturated with the antibiotic is placed on the lawn. The antibiotic diffuses into the medium at the same time that the bacteria are trying to grow. If the bacteria are susceptible, an area of clearing called the “zone of inhibition” will be seen in the lawn surrounding the disks at the end of the incubation period. The definition of susceptibility and resistance varies with the type of test—either the bacteria are observed to grow right up to the edge of the antibiotic disk, or a small zone of inhibition that falls within a measured size range is seen. The agar plate in Figure 1 shows variations in the size of the zones of inhibition for four antibacterial chemicals. For the Kirby-Bauer assay, the size of each zone must be carefully measured.
As demonstrated, prepare suspensions in sterile saline to match a 0.5 McFarland standard using the bacteria listed below. For each, also indicate if they are Gram-positive or Gram-negative.
Escherichia coli ___________________________________
Staphylococcus aureus ___________________________________
Pseudomonas aeruginosa _________________________________
Once made, the three standardized suspensions of these bacteria will be used again later in this lab, so do not immediately discard them.
For uniformity across labs, the same type of medium must be used by each lab. The standard method calls for Mueller-Hinton agar (MHA) plates, which is a special formulation prepared with a lower concentration of agar at a specific pH to facilitate diffusion of the antibiotics into the medium.
Obtain three MHA plates, and as demonstrated, inoculate each with one of the bacteria listed above, using a sterile swab soaked in the corresponding bacterial suspension.
Using forceps sterilized in alcohol, place one disk of each antibiotic to be tested on all three of the inoculated plates, far enough away from each other so that the potential zones of inhibition will not overlap.
The standard method calls for the plates to be incubated at a temperature range of 35°C ± 2°C for 18–24 hours. This may be modified to accommodate your laboratory schedule, as directed by your instructor. Make a note of the time and temperature for incubation if it is a modification of the standard method, below:
Incubation time and temperature: ____________________________________
The four antibiotics we will be testing have different cellular targets, and therefore bacterial responses to them will vary. The bacterial cell wall is often a target of disruption for antibiotics. Two of the bacteria above have the same Gram stain reaction, but Pseudomonas spp. generally have a broader range of resistance than other types of bacteria. Research, and then below, list two strategies employed by pseudomonad bacteria to resist destruction by antibiotics:
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
Complete the table below with the mechanism of action for each of the antibiotics we’ll be testing. Also, use a website such as Drugs.com or Rxlist.com to research the medical use (indications for use) for the antibiotic, and include that information in the table.
| Antibiotic | Bacterial cell target/
Mechanism of action |
Indications for use | Contraindications for use (including side effects) |
| Cefixime
(Suprax) |
|||
| Tetracycline
(Panmycin) |
|||
| Azithromycin (Zithromax) | |||
| Ciprofloxacin (Cipro) |
After incubation, look for zones of inhibition around each disk in all three lawns. If a zone is observed, measure the diameter in mm using a metric ruler and record the measurement in the table below. Using the table of standard values (Table 1), compare the measured size of the ZOI and determine if the zone size indicates the bacteria are resistant, susceptible, or have an intermediate susceptibility to each of the antibiotics.
| E. coli | S. aureus | P. aeruginosa | ||||
| Antibiotic | ZOI in mm | Result | ZOI in mm | Result | ZOI in mm | Result |
| Cefixime | ||||||
| Tetracycline | ||||||
| Azithromycin | ||||||
| Ciprofloxacin | ||||||
Based on what you learned about each antibiotic in terms of its medical uses and patterns of susceptibility, consider which of the four antibiotics tests you would prescribe for the following types of infections, if you were the medical professional in charge of the case:
A urinary tract infection (UTI) caused by E. coli
A wound infection caused by S. aureus ____________________________________________
A respiratory tract infection caused by P. aeruginosa __________________________________
Using the Disk Diffusion Method to Test Chemicals for Antibacterial Action
The basic principles of the Kirby-Bauer method can also be applied to investigate the antimicrobial properties of solutions with known or suspected actions against bacteria.
Disinfectants and antiseptics are chemicals used for microbial control in many settings. As with antibiotics, microorganisms differ substantially in their susceptibility to the chemical agents we use to reduce the number of microbes on inanimate surfaces (disinfectants) or living tissues (antiseptics). To evaluate their potency, effectiveness is compared to that of a standard disinfectant such as phenol, which was the chemical first used and endorsed by Joseph Lister for aseptic surgery. This type of comparison can be done using broth dilution methods, but may also be accomplished by disk diffusion assay, in which the effectiveness of a particular chemical agent is assessed in a direct comparison of the size of the zone of inhibition to a positive control like phenol, which has a known and powerful antibacterial effect.
Obtain three MHA plates and label each plate with the name of one of the test bacteria (E. coli, S. aureus, and P. aeruginosa). Using the 0.5 McFarland-adjusted cell suspensions made previously, prepare lawns of the three bacteria on the surface of the MHA plates.
Available in lab will be several samples of chemicals with known or suspected antimicrobial properties. Choose three that you would like to investigate, and list your choices below. If the agent is a commercial product, also list the “active ingredient” from the label of the product. Also, record the positive control you will be comparing your selections against, according to your instructor.
| Chemical Agent | Active Ingredient (if known) |
| Positive Control | Active Ingredient |
On the bottom of the Petri dish holding the bacterial lawns, use a marker to draw intersecting lines that divide the plate into four sections. Label one section (+) to represent the positive control. Label the three other sections with the name or abbreviation of the test chemicals you selected.
Using forceps sterilized in alcohol, remove a sterile filter paper blank disk from its container and soak it in the positive control solution. Remove it from the solution and allow the excess liquid to drip back into the container. Place the soaked disk in the center of the appropriately labeled section on one of the plates, and then repeat the process for the other two plates.
Once the positive control disks have been placed, soak blank disks in the test solutions you chose and place them on the three lawns. Use the same three test solutions on each of the lawns.
Incubate the plates (overnight at 37°C is preferred). After the incubation period, examine the disks in the lawns for a zone of inhibition. Measure the diameter of the ZOI for the positive control first, as this is the standard by which you will be assessing the effectiveness of the test solutions. Record your results in the table below.
| Solutions tested (write name) | E. coli | S. aureus | Ps. aeruginosa |
| Pos. control _______________________ | |||
| Test 1 _________________________ | |||
| Test 2 _________________________ | |||
| Test 3 _________________________ |
List the chemical agents you tested that were at least as effective against each bacterium as the positive control:
Bacteria Effective test chemicals
E. coli ____________________________________________
S. aureus ____________________________________________
P. aeruginosa ____________________________________________
Of the chemical agents you tested, which one shows the greatest overall range of antibacterial action?
__________________________________________________________________________
__________________________________________________________________________
Which bacteria showed the greatest degree of resistance to the chemical agents tested?
__________________________________________________________________________
Were any of the results a “surprise” to you (for example, perhaps something you thought would be a good disinfectant was not, or one of the natural products tested was more effective than predicted?). Reflect below, and you may be asked to share your thoughts on this during a discussion of the results.
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
__________________________________________________________________________
Using Antibiotic Susceptibility for Bacterial ID
Browsing through Bergey’s Manual reveals that susceptibility or resistance to various antibiotics can be useful when it comes to discriminating between bacterial species. Two examples are the novobiocin resistance test for Staphylococcus spp. and the “Taxo A” or the bacitracin susceptibility test for Streptococcus spp.
Novobiocin resistance test
This test was originally developed as a test to identify S. saprophyticus, which is a coagulase-negative staphylococci and the second most common cause of urinary tract infections (after E. coli). After the procedure has been demonstrated, perform the test using the cultures of Staphylococcus aureus and Staphylococcus saprophyticus provided.
Prepare standardized suspensions of S. aureus and S. saprophyticus, by transferring 2 ml of sterile saline to a culture tube, then adding colonies until the turbidity (cloudiness) in the solution matches that of a 0.5 McFarland optical standard.
Obtain one Mueller-Hinton agar (MHA) plate, and on the bottom of the Petri dish, draw a line with a marker to divide the plate in half. Label each half with the name of one of the two staphylococci.
Soak a sterile swab in one of the bacterial suspensions, and transfer it to the appropriately labeled side of the divided plate. Spread the suspension to create a confluent layer of bacterial cells which will grow into a lawn of bacterial colonies. Repeat the process with the other bacterial suspension on the other half of the plate.
With forceps sterilized in alcohol, place one novobiocin disk (5 µg) in each of the two lawns. Incubate the plate for a minimum of 24 hours. After incubation, examine the lawn around each disk. If a zone of inhibition is noted, measure the diameter of the zone with a metric ruler, in mm. For this test, bacteria are considered positive for novobiocin resistance if there is no zone of inhibition, or if the zone size is less than 12 mm. Susceptibility is a negative test. Record your results below.
| Bacteria | ZOI diameter (mm) | Susceptible or Resistant? | Positive or Negative outcome |
| S. aureus | |||
| S. saprophyticus |
| Table 1. Table of Standard Values: Kirby-Bauer Disk Diffusion Test | |||||
| Antibiotic | Spectrum | Disk | Zone diameter nearest whole mm | ||
| Resistant | Intermediate | Susceptible | |||
| β-LACTAMS (penicillins) | |||||
| Carbenicillin | Pseudomonas | 100 µg | <13 | 14-16 | >16 |
| Gram negatives | 100 µg | <19 | 20-22 | >23 | |
| Methicillin | Staphylococci | 5 µg | <9 | 10-13 | >14 |
| Mezlocillin | Pseudomonas | 75 µg | <15 | >16 | |
| Other Gram negs | 75 µg | <17 | 18-20 | >21 | |
| Penicillin | Staphylococci | 10 units | <28 | >29 | |
| Enterococci | 10 units | <14 | >15 | ||
| Piperacillin | Pseudomonas | 100 µg | <17 | >18 | |
| Other Gram negs | 100 µg | <17 | 18-20 | >21 | |
| β-LACTAM/ β-LACTAMASE INHIBITOR COMBINATIONS | |||||
| Amoxycillin/clavulanate | Staphylococci | 20/10 µg | <19 | >20 | |
| Other organisms | 20/10 µg | <13 | 14-17 | >18 | |
| Piperacillin/tazobactam | Pseudomonas | 100/10 µg | <17 | >18 | |
| Other Gram negs | 100/10 µg | <17 | 18-20 | >21 | |
| Staphylococci | 100/10 µg | <17 | >18 | ||
| CEPHALOSPORINS | |||||
| Cefotaxime | 30 µg | <14 | 15-22 | >23 | |
| Cefixime | 30 µg | <15 | 16-18 | >19 | |
| Ceftriaxone | 30 µg | <13 | 14-20 | >21 | |
| Cefuroxime oral | 30 µg | <14 | 15-22 | >23 | |
| CARBAPENEMS | |||||
| Imipenem | 10 µg | <13 | 14-15 | >16 | |
| MONOBACTAMS | |||||
| Aztreonam | 30 µg | <15 | 16-21 | >22 | |
| GLYCOPEPTIDES | |||||
| Vancomycin | Enterococci | 30 µg | <14 | 15-16 | >17 |
| Other Gram pos | 30 µg | <9 | 10-11 | >12 | |
| AMINOGLYCOSIDES | |||||
| Gentamicin | 10 µg | <12 | 13-14 | >15 | |
| Streptomycin | 10 µg | <11 | 12-14 | >15 | |
| Tobramycin | 10 µg | <12 | 13-14 | >15 | |
| MACROLIDES | |||||
| Azithromycin | 15 µg | <13 | 14-17 | >18 | |
| Clarithromycin | 15 µg | <13 | 14-17 | >18 | |
| Erythromycin | 15 µg | <13 | 14-22 | >23 | |
| TETRACYCLINES | |||||
| Doxycycline | 30 µg | <12 | 13-15 | >16 | |
| Minocycline | 30 µg | <14 | 15-18 | >19 | |
| Tetracycline | 30 µg | <14 | 15-18 | >19 | |
| QUINOLONES | |||||
| Ciprofloxacin | 5 µg | <15 | 16-20 | >21 | |
| Nalidixic acid | 30 µg | <13 | 14-18 | >19 | |
| Norfloxacin | 10 µg | <12 | 13-15 | >16 | |
| Ofloxacin | 5 µg | <12 | 13-15 | >16 | |
| OTHERS | |||||
| Chloramphenicol | 30 µg | <12 | 13-17 | >18 | |
| Clindamycin | 2 µg | <14 | 15-20 | >21 | |
| Nitrofurantoin | 300 µg | <14 | 15-16 | >17 | |
| Rifampin | 5 µg | <16 | 17-19 | >20 | |
| Sulfonamides | 250/300 µg | <12 | 13-16 | >17 | |
| Trimethoprim | 5 µg | <10 | 11-15 | >16 | |
| Trimethoprim/ sulfamethoxazole |
1.25/ 23.75 µg |
<10 | 11-15 | >16 | |
| Note Adapted from: Clinical Laboratory Standards Institute. (2006). Performance standards for antimicrobial disk susceptibility tests; Approved standard 9ed. CLSI document M2-A9. 26:1. Clinical Laboratory Standards Institute, Wayne, PA. | |||||

