2 Working Effectively with Home Care Clients
Introduction
All of us have unique needs and backgrounds. We look different from each other; we have different cultural backgrounds, religions, ages, social classes, financial statuses, occupations, interests, and families. We may speak different languages. We have different values, or thoughts on what is important to us. What makes each of us the same, each human being the same as the next, is that we have the same basic physical and psychological needs. This module will explore the basic physical and psychological needs of humans. It will also look at how culture influences people’s behavior, values, and health care practices. You will gain some basic information about a variety of cultures and religions with whom you may work if you choose to pursue a career as a Home Health Aide/Personal Care Aide. During this module, you will learn a variety of Communication skills to use in working with patients, and how to best develop a positive working relationship with patients. We will also explore how to document observations and the work done with patients. Finally, you will learn about the different types of abuse, the signs to look for, and how to report suspicions of abuse. We will also discuss the importance of patient rights and how best to support the rights of patients.
Unit A: Human Needs, Culture & Diversity
Maslow’s Hierarchy of Needs
We all need oxygen, food, water, sleep, and a safe shelter. We all also have psychosocial needs, which involve our social, emotional, intellectual, and spiritual needs. These needs may differ from one person to the next; but we all have them. When our needs go unmet, we may react in different ways. Some people become depressed, some anxious, some afraid, and some may even become angry and lash out at the people around them. When people become stressed, their physical health also is affected, and physical problems that could lead to illness may develop.
Without meeting basic human needs, a person cannot develop to their fullest potential. Home Health Aides/Personal Care Aides are in a unique position to help the people they work with. These individuals help them to meet their physical, emotional, mental, social, and spiritual needs so that patients can live to their fullest potential.
Abraham Maslow was a researcher of human behavior. He developed the Maslow’s Hierarchy of Needs. This model shows us the importance of the physical and psychosocial needs of humans. The needs are arranged in a hierarchy, which means they are arranged in order of importance. Maslow’s Hierarchy of Needs is arranged in what looks like a pyramid made up of five levels of needs. Maslow believed that people must meet the needs at the bottom of the hierarchy before they can successfully meet the next higher up need.
These needs include: Physical Needs, Safety and Security Needs, Need for Love and Belonging, Need for Self-esteem, and Need for Self-actualization. Let’s explore what each of these levels means and how Home Health Aides/Personal Care Aides can help their patients achieve their needs at each level of Maslow’s Hierarchy of Needs.
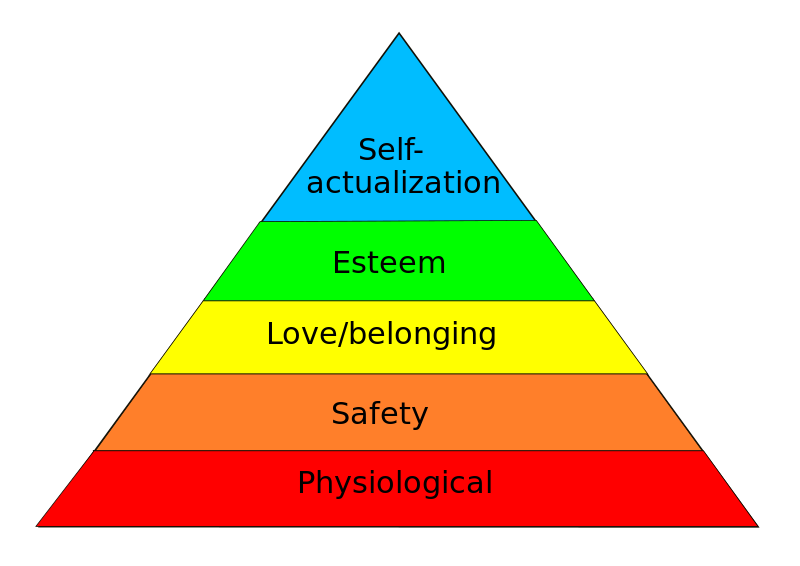
Physical Needs
At the most basic levels of Maslow’s Hierarchy of Needs are our physical needs. These needs include oxygen, food, activity, sleep, and elimination. These are the basic needs humans must meet in order to survive. Maslow believed that these needs must be met first before a person can go on to meet other needs, such as their psychosocial needs. Home Health Aides/Personal Care Aides, work to help their patients meet their basic physical needs. They assist them in completing Activities of Daily Living (ADLs), such as eating, drinking, toileting, bathing, and grooming. Taking vital signs, shopping for and preparing food for their patient, and measuring intake and output are other important tasks that Home Health Aides/Personal Care Aides do to help patients meet their physical needs.
Safety and Security Needs
After meeting our basic physical needs, according to Maslow’s Hierarchy of Needs we must have our safety and security needs met. This includes having a safe place to live and to not feeling afraid within our homes, or of the people around us. Home Health Aides/Personal Care Aides work within the patient’s environment to make their home safe so that their patient feels safe. This means they will need to ensure that there are no hazards in the patient’s home such as clutter or loose rugs that could cause a patient to slip, trip, or fall. Checking to ensure safety and grab bars are secure to the wall and that non-slip tub mats and shower chairs are used ensures a safe environment for their patient. Keeping the patient’s home clean and free from dirt by completing tasks such as laundry, vacuuming, and cleaning, maintains a safe environment for their patient. Ensuring that their patients properly use assistive devices such as canes and walkers also ensures their safety. Helping patients to meet their safety needs also includes taking care to properly wash hands and to wear gloves as appropriate, in order to prevent the spread of infection. When people are sick or who may not be as independent as they used to often feel afraid. The job of a Home Health Aide/Personal Care Aide is to help them feel secure by reassuring them, being patient when they try to complete tasks on their own, and being competent (good) in the tasks they complete.
Need for Love and Belonging
Once people have met their physical and safety/security needs, the need for love and belonging is the next important level in Maslow’s Hierarchy of Needs in order for us to grow and flourish as humans. This need includes feeling that we are loved and cared for. Humans need to feel important to other people and to feel that they are a part of something, such as a family or community.
For Home Health Aides/Personal Care Aides, the way they care for their patients demonstrates to them that they care for and about them. This means being patient, kind, compassionate, understanding, trustworthy and accepting the patient’s thoughts, feelings, and uniqueness, even if they do not agree with them.Home Health Aides/Personal Care Aides can ask patients to share their memories and stories with them to help the patient recognize the importance they have in others’ lives.Family is an important part of a patient’s life and helps them to meet their need for love and belonging. We all have different views of what “family” means to us. Individuals must be careful not to judge who a patient considers part of their family. Family means everyone the patient sees as part of their family. Include the patient’s family in their care if they wish for them to be involved.
Spirituality and religious practices may also be important parts of the patient’s life. Helping patients meet their spiritual and religious needs may help them to cope with an illness or disability. Remember that each of us has our own unique spiritual and religious views. It is important not to judge the beliefs of others and to allow the patient to practice what they believe. If a patient has particular dietary restrictions due to their religious belief, a Home Health Aide/Personal Care Aide must be sure to accommodate these. They must also allow their patient to have privacy to pray, practice religious rituals, and to have time for clergy visits. If asked, they may read aloud religious materials and sit with their patient as they pray. A person does not have to believe in their particular religion in order to be respectful and to support a patient’s beliefs.
Need for Self-esteem
The need for self-esteem is the next level in Maslow’s Hierarchy of Needs. Self–esteem involves valuing and respecting oneself. Self-esteem comes from within us, and from interactions and feedback from other people. When people become sick, injured, or disabled, their self-esteem may be affected. They may not see themselves the way they used to.They may have concerns about their appearance or physical disability. They may feel that others do not see them as a whole person. They may worry that others see them less than they used to be or what they could be due to limitations from their physical or mental disability. A Home Health Aide/Personal Care Aide can help patients to accept physical changes by demonstrating acceptance. This means they must watch their body language while caring for patients. There may be situations where a patient has an injury or wound which may be difficult to look at. It is important to remember that the patient is watching for a reaction. Showing that they are okay with the patient’s physical changes will tell the patient that they are accepted exactly the way they are.
It is important to treat each patient as a unique individual with talents and strengths. Sometimes, people forget that they still have value as a person when they are sick. Home Health Aides/Personal Care Aides should get to know their patients to find out who they are as a person. Understanding their patients will allow the Home Health Aides/Personal Care Aides to help the patients see how valued they are. Home Health Aides/Personal Care Aides can also help to increase a patient’s self-esteem by allowing them to be as independent as possible, providing encouragement when they are doing a task they have difficulty with, and giving praise when they are successful. Demonstrating that they value the patient’s feelings, values, and their beliefs also helps to increase a patient’s self-esteem.
Need for Self-actualization
The need for self–actualization is the highest level of Maslow’s Hierarchy of Needs. Self-actualization means that we try to be the best person that we can be and try to reach our full potential. We each have different views of what being our best person means and what reaching our full potential means. It is important to remember to respect a patient’s thoughts and goals. The goals that we each set often change throughout our lives and may change as a result of experiencing an injury, illness, or disability. As a Home Health Aide/Personal Care Aide, it is important to accept others the way they are. Home Health Aides/Personal Care Aides are also in a position to help their patients work to accept themselves and to set and work towards new goals.It is important to remember that what a HHA/PCA views as a good goal may be different from the goal the patient wants to set. Using good communication skills is important to help patients work towards realistic and achievable goals.
Self-Check Activity m2-1
Self-Check Activity M2-1
Match the HHA/PCA’s task to the appropriate level of Maslow’s Hierarchy
| Task | Level of Maslow’s Hierarchy |
| 1. Allow a patient time to pray before they eat if they want ______ | a. Physical Needs |
| 2. Assist with eating and dressing ________ | b. Safety/security Needs |
| 3. Help a patient to set and meet their goal of putting their shoes on independently ______ | c. Love/Belonging Needs |
| 4. Teach a patient to correctly use their walker _________ | d. Self-esteem Needs |
| 5. Giving praise to a patient when they can do a task such as put on their shoes, which they have not been able to do since injured _________ | e. Self-actualization Needs |
Diversity
Culture
Culture is a set of behaviors, beliefs, values, attitudes, and goals shared by a group of people. Our culture is a powerful part of what makes us who we are and how we live. Groups of people such as families, friends, religious groups, and organizations all share a culture. Rules in a culture can be expressed by spoken and unspoken ways, such as whether direct eye contact or shaking of hands is considered to be appropriate. Many characteristics make up cultures and most people belong to numerous cultures. Race, spiritual/religious beliefs, national origin (the country the person comes from), sexual orientation, and age make up various cultures. People often identify themselves or define who they are based on their cultures.It is important to remember that we often belong to a number of cultures, and one aspect of our culture does not solely define us. It is also important to remember that one culture is not better than another. Health care workers need to try to understand what cultures a patient belongs to and what customs within those cultures the person believes or practices. This helps them to better understand where their patient is coming from and to better take care of them.
Race versus Culture
Race is not the same as culture. Race is a classification of people based on physical attributes, geographic ancestry (where a person came from originally), and inherited characteristics. In the United States, for example, some races are: White American, African American, Native American and Alaska Native, Asian American, and Native Hawaiian or Pacific Islander. Some people may identify as being multi–racial, meaning they have more than one race. We often identify ourselves as being a part of a particular race, but this is not the only aspect of who we are. It is important to be careful to not judge people by their race, or what you think their race is. This is called racism. Racism is a belief that one racial group is better than another racial group, or that one member of a race is the same as all other members of that race. Racism results in prejudice against a particular race.
Ethnocentrism, Diversity, & Stereotypes
In working with others, we must be careful of ethnocentrism. Ethnocentrism is thinking that your culture and beliefs are superior to, or better than another person’s. All of our cultures are equally important. No one culture is better than another. The various cultures bring diversity to our world. Diversity means including and respecting different types of cultures. We must also be careful of stereotypes. Stereotypes are when you believe that all people within a group are the same based on what you know about one individual within a group. Stereotypes can be about any characteristic of a person such as their looks, sexual orientation, weight, or behavior. We often learn stereotypes from the media and from our families as we are growing up. For example, until recently it was believed that all women should stay at home to cook, clean, and care for their children. As a result, people may have stereotypes about women, such as, “All women are good cooks”, or “Women should be secretaries and men bosses.” Stereotypes are very harmful to people. They can make us feel misunderstood and not respected. It is important to become aware of the stereotypes you have about others so that you do make a patient feel that they are not respected or valued.
Self-Check Activity M2-2
| 1. “Men should not show their emotions by crying in front of others.” | A. Ethnocentrism |
| 2. “Everyone who comes to the United States should learn to speak English.” | B. Stereotype |
| 3. “I identify myself as a Native American. This is my ______.” | C. Culture |
| 4. “I am Italian. This is my________” | D. Race |
| 5. “The agency I work for hires people of all genders, races, ages, and cultures.” | E. Racism |
| 6. “The agency I work for will only hire Caucasians.” | F. Diversity |
Self-Awareness
Take a moment to think about what makes up your culture. What groups do you consider to be important to you? What roles do you play in your life? Are you a mother, father, daughter, or grandson? Do you have religious or spiritual beliefs that you practice? Do you have traditions and rituals in your family that are important to you? How do you identify yourself? What groups do you belong to? Do you have hobbies, clubs, organizations, or a profession to which you belong to and identify with?
Your culture is a part of who you are. It has helped to shape your beliefs, values, and attitudes. You bring it everywhere with you. You bring your culture to work with you. Your culture influences how you view and interact with the world around you. It influences how you understand and care for your patients. It is important to engage in self–reflection in order to better understand how you see yourself. The more you understand your own beliefs, the better able you will be to understand and appreciate the beliefs of others and to care for patients if you pursue a career as a Home Health Aide/Personal Care Aide.
Self-Awareness Activity
This activity will help you gain a better understanding of the different ways you identify yourself. Begin by drawing a large circle in the center of a piece of paper. Then, draw lines from that center circle. Draw smaller circles at the end of each of those lines. In the center circle, write the role, identity, or culture that is most important to you and by which defines who you are. For example, it might be your name, gender, race, ethnic heritage, religion, profession, a role in your life that is crucial to your identity, or any other aspect of your identity that is the center to who you are. In each of the smaller circles, write down all the other roles or cultures to which you belong, or other aspects of your life that help identify who you are. The smaller circles may have words that describe your identity such as mother, daughter, health care aide/personal care aide, student, musician, writer, Irish, African, Catholic, Muslim, etc. The possibilities are endless.
After you complete your circles, take a moment to think about what each of the identities means to you.How do they shape how you view the world? Do you think that others could have stereotypes about any of the aspects of your identity? If so, what would this mean to you? How would you go about challenging those stereotypes to help the other person understand who you really are? Then, think about other people you may know. What do you think would be in their circles? Do you have stereotypes of any of other roles, cultures, and important aspects of other people’s identities?
This activity will help you to understand how diverse your own beliefs, customs, and roles are. It will help you to see how various roles are important in your life and how others may view your own differences. This will help you to become more understanding of the uniqueness of each patient with whom you may work if you choose to pursue a career as a Home Health Aide/Personal Care Aide.
Cultural Awareness & Cultural Competence
Cultural awareness means how aware you are about the values and beliefs of other cultures. It is also means how much you appreciate the various aspects of the different cultures. Becoming culturally aware is a lifelong journey. It is nearly impossible to know all the customs and beliefs of every culture in the world. What is important for health care workers is to strive to learn as much as they can about the variety of cultures in our world. For each patient that they work with, they should ask them to tell them about their cultural beliefs and practices. In this way, they will always be learning about all the different cultures, and working to better understand and care for their patient!
Cultural competence goes along with cultural awareness. Cultural competence means the ability to incorporate cultural awareness into the health care practice. It means understanding and respecting a patient’s cultural beliefs and working with them in a way to demonstrate that you respect and honor these beliefs. For example, if a patient likes to pray before eating meals, and the Home Health Aide/Personal Care Aide provides and supports their prayer prior to their meals, they are practicing in a culturally competent manner. The more aware they become of different cultures, and the more they learn to appreciate differences, the more culturally competent they will become.
Self-Check Activity M2-3
Directions: Fill in the blank with the correct term that matches the description
1. This term means providing healthcare in a way that demonstrates you understand, honor, and respect your patient’s cultural beliefs _______________________________.
2. This term means learning about the values, beliefs, and practices cultures that are different than your own ______________________________.
Cultures
In this next section, we will explore some common cultures. Please note that this discussion of cultures is not comprehensive, meaning that there are many more cultures than those listed here. Remember also that the information here is to be used as a guide. Each person is unique. The information here is to provide some basic knowledge about the culture. It is also not intended to mean that just because a person is from one of the cultures listed here that they necessarily share the customs and beliefs described. It is important for the Home Health Aide/Personal Care Aide to get to know their patient, their beliefs, traditions, and values. It will make all the difference in their work with them and will lead to a positive working relationship! To learn more about various cultures and healthcare practices, please visit Dimensions of Culture: Cross-cultural communications for Healthcare Professionals at: http://www.dimensionsofculture.com/
African American
Africa is a continent that has dozens of different tribes, ethnic, and cultural groups, with hundreds of different languages and dialects spoken. A person may define themselves as “African” if they live in or come from one of the African countries.The term “black” is usually defined as people who descended from an African country (Carteret, 2011b).The term “African American” can be defined as ‘blacks” who are born in the United States but who descended from the African continent (Carteret). Depending on family and cultural values and beliefs, people may prefer one term over the other as a way to identify themselves. Learn the terms a patient chooses to use to define their identity. It is important to remember that people cannot be defined by their skin color, as there are a variety of skin tones, from light to dark of people who define themselves as African American (Carteret). Remember, a shared complexion does not necessarily mean there is a shared culture. It is important to find out the terms a patient uses to define their identity.
The African American family may include extended family and people outside of the biologic family, or “fictive kin” (Carteret, 2011b). Elders are highly respected, with the woman often taking on a matriarchal role, although decision making may be done by either the mother or father. Families tend to avoid placing loved ones in long-term care facilities and instead care for their elders or disabled family members in the home (Carteret).
African Americans often have ties to a religious community, with many having a Christian faith or following Islam (Carteret, 2011). Additionally, according to Carteret, during times of illness and impending death, many African Americans often turn to their faith. It is important to find out a patient‘s’ religious or spiritual beliefs and to honor these. Carteret also writes that it is often important for extended family and friends to be present to gather around their loved one during times of imminent death (death that is likely to happen soon) and that effort to inform and allow extended family to be present should be made.
Due to the historical mistreatment of African Americans in healthcare, they may be mistrustful of healthcare providers and reluctant to participate in treatment or share personal issues (Carteret, 2011b). It is very important to work on building trust while providing health care.
Self-Check Activity M2-4
True or False?
1. Many African Americans have a strong sense of family and spiritual faith. Those considered family may be outside of their family of origin and include close friends, or “fictive kin”.
2. You can use the term “black”, “African”, or “African American” to describe any person of color.
Asians
The term Asian is a general term for many different cultures that originate in an Asian country. According to Carteret (2010a, 2010b), Asian cultures include people from various Asian countries and may be delineated by the specific Asian country from which they live or originate. People who consider themselves to be Asian may be Pacific Islanders (from Hawaii, Samoa, or Guam), Southeast Asians (from India, Vietnam, Thailand, Cambodia, Laos, Burmese, and Philippines), and East Asians (from China, Japan, and Korea). Each of these cultures has many different beliefs, norms, and traditions. It is important to not generalize from one Asian culture to the next. Get to know the patient and their beliefs and customs.
Generally speaking, Asians tend to be group and family oriented (Carteret, 2010a). This is known as a collectivist culture. Different from the typical individual oriented culture in the United States, decisions and actions are made as part of a group and with consideration to the effects on the group. Loyalty is very important to the family and family members’ behaviors are a reflection of the honor and respect shown to the family. Therefore, decisions are often made with the effects on the family in mind and it is important to take care not to disgrace oneself or one’s family (Carteret).
Self-control is also important; expression of intense emotion such as crying, yelling, pain, or grief may not be shown (Carteret, 2010a). Many people from Asian cultures may not be direct in conversation, and may see such directness as rude. Many Asians may smile when confused or embarrassed, which can be mistaken as a sign of pleasure or understanding (Carteret). Similarly, many Asians may also nod during conversation, which can also be mistaken as understanding during conversations about health care concerns and treatment. It is important to try to determine if a patient truly understands the situation. According to Carteret, Asian cultures typically take the context of the situation in mind. This means that they pay careful attention to nonverbal cues during conversation such as gestures, tone of voice, eye contact, and silence. It is important to remember to pay attention to the nonverbal cues you are using and to try to understand those that are being Conveyed (said) by a patient. Much of the meaning of what is being conveyed (said) can be found in the nonverbal cues rather than the verbal words in Asian patients.
Many Asians believe in fatalism, or the belief that nothing can be done about a situation or one’s healthcare; it is decided by fate or karma. This may make Asian patients and families appear to be “resigned to their situation” (Carteret, 2010a). It is important to take care when discussing a health care situation or disease in how it is presented. While in the United States we often look at healthcare in terms of fighting a disease, Asian patients may not look at seeking treatment in this way. There also may be many healthcare practices outside of what Western medicine considers treatment, which are unique to each Asian culture.
Many Asian cultures focus on the holistic treatment or treating both the body and mind, while Western medicine tends to only focus on treating the body. Herbal remedies and the use of acupuncture may be health care practices of many Asian patients (Carteret, 2010b). It is important if Home Health Aides/Personal Care Aides become of aware of the use of herbals and other medicines that they report these to their supervisor. While it is important to respect and honor cultural practices of patients, it is also important that the healthcare team knows which practices are being used. There are some herbs for example that interact with Western medications. Some Asian cultures also practice a technique called cupping, in which a glass or plastic cup is pressed against the skin, creating a vacuum in order to relieve the patient of pain and to treat respiratory diseases (Carteret. If Home Health Aides/Personal Care Aides become aware of areas on their patient’s body such as burns or circles, it is important to ask the patient, in a non-judgmental way to explain them and then they should discuss findings with their supervisor.
Self-Check Activity M2-5
True or False
1. When working with Asian patients, it is generally important to pay attention to nonverbal cues, such as nodding, smiling, tone of voice, and gestures during conversations. __________
2. Many Asian cultures are collectivist, meaning they consider how their individual decisions will impact their whole family, so health care decisions and treatments should be focused on the family as a whole. _______________
Latinos
The term Latino means a person whose origins are from a Spanish-speaking country, such as: Caribbean, Mexico, South America, and Central America (Carteret, 2011a). Latinos often have a very deep sense of family connection, called familismo. These family members include extended members of the family and close friends whom they trust; they may be slow to trust outsiders (Carteret, 2010f; 2011a). Family members, including extended members of the family such as grandparents, aunts and uncles may be very involved in the healthcare of the patient, and want to be present to help make healthcare decisions (Carteret, 2010f). It is very important to include all members of the family during health care decision making and care provision. This will help the patient and family to trust the health care worker and be willing to work with them.
Latinos are traditionally very focused on relationships (Carteret, 2011a). As such, it is important for Home Health Aides/Personal Care Aides to take their time during the provision of care, demonstrate warmth, touch, concern, friendliness, and a sense of confidence. Latinos feel great respect for physicians and healthcare providers as they believe in the importance of respect, or respecto, so may not want to question health care providers (Carteret). This could result in not understanding healthcare treatment. Respect is very important for many Latinos. According to Carteret, Latinos may expect a “formal friendliness” from their healthcare providers. They may expect to be greeted and say goodbye with a handshake and “good morning/afternoon.”They may also prefer a more formal address, such as “Mr. or Mrs.” in conversation.The concept of hierarchy in a Latino family is another aspect that healthcare providers should be aware of to ensure they are demonstrating respect for the family.
In the presence of other family members or a husband or wife, all members should be greeted in such a way to demonstrate respect. This includes greeting family members as “Mr. or Mrs.” The oldest male of the family often has the greatest power of the family and decisions may be deferred to him (Carteret, 2011a). The concept of machismo means male Latinos are expected to be providers of the family and uphold the honor of their family. As such, female Latinos may defer decisions to their husbands or take on a more submissive role. Healthcare providers should be aware of this and ensure that healthcare decisions are also discussed with the head of the household.
Latinos may also have different concepts or health and healthcare practices from traditional healthcare practices. Latinos often believe that life is full of uncertainty and that there is not much they can do to alter the course of their life (Carteret, 2011a). This belief is called fatalism, which means there is little they can do to alter the course of their fate. This may result in delaying treatment or healthcare seeking behaviors.
Latinos may have many folk beliefs which influence their healthcare decisions and practices. Many Latinos may believe that people who suffer from physical illness do so because of an illness of emotional or spiritual origins (Carteret, 2010b). For example, some Latinos believe illness of a child may be caused by an evil eye or Mal de Ojo (Carteret). The belief is that someone who strongly admires and wants the child has placed a spell on the child, resulting in illness. It is common for parents to place an amulet, or a azabache on the child in the form of jewelry to protect them against Mal de Ojo (Carteret). Additionally, Carteret describes a practice common to Latinos where a folk healer may treat the child by passing an egg over the child and placing it under the child’s pillow at night; if the egg cooks, then the child had Mal de Ojo.
Self-Check Activity M2-6
True or False
1. For many Latinos, there is a strong sense of family, or familismo, in which health care decisions and treatments involve the entire family, including extended family members. _________
2. It is important for many Latinos that healthcare providers show respect, or respect and greet all members of the family at the start and end of healthcare encounters. _____________
Middle East
Countries associated with the Middle East traditionally include: Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Palestine, Saudi Arabia, Syria, Turkey, and Yemen to name a few. People from the Middle East traditionally have a strong sense of affiliation with their family. Families and friends may be very close-knit and involved in the healthcare of the patient, with the elder member of the family expecting to be involved in health care decisions (Carteret, 2010c). Because of the close connection among those considered to be part of the patient’s close-knit circle, members of the family may have “doubt about the intentions of those outside their intimate circle” (Carteret). Healthcare providers may need to provide reassurance about having their family members’ needs taken care of. They must also take care to be cognizant (aware) of gender differences.
People of the Middle East may often prefer to have same-sex caregivers and have the eldest member of the family or the husband answer questions and make decisions for female patients (Carteret, 2010c). Additionally, according to Carteret, direct eye contact with members of the opposite sex is frowned upon. Middle Easterners may touch more frequently and tend to have a closer personal space during conversation than those from Western cultures (Carteret). However, take care to remember gender differences, as too-direct contact, for example between a male healthcare provider and a Middle Eastern female may be seen as a sign of sexual interest. As such, male Middle Easterners may have difficulties interacting with females who are in a position of authority, such as female physicians.
Middle Easterners generally value Western medicine but may have some folk beliefs such as illness being caused by the Evil Eye, or a person who is jealous, which causes the illness the patient is experiencing (Carteret, 2010c). Further, according to Carteret, Middle Easterners may also follow special diets and may not eat certain foods together at the same meal. Foods may be considered “hot” or “cold”. People of the Middle East may resist going to the hospital as it is seen as a place where people die (Carteret). They may also be concerned that their loved one will not be cared for after death according to religious customs. Mourning for the death of a loved one is often loud and with great emotion expressed, as this is a sign of respect (Carteret).
Self-Check Activity M2-7
True or False
1. When working with Middle Eastern patients, it is a good idea to check to see if there are gender preferences for whether the patient would prefer to have a male or female to provide their care. ______
2. It is not important to consider the family as part of the healthcare team when working with Middle Eastern patients. __________
Religions of the World
There are numerous religions and spiritual beliefs throughout the world. Religious beliefs influence people’s values, morals, behaviors, and traditions. Religion may be important to some people and unimportant to others. Some people consider themselves to be spiritual, but may not practice or be affiliated with a particular religion. Other people do not believe in any religion or God. Only some of the more common religions are discussed here. Remember, even if a patient practices one of the religions discussed, they may or may not adhere to the beliefs or practices described. Always ask a patient what their individual beliefs and practices are.
Agnostics and Atheists
Agnostics are people who do not know if there is a God. They do not necessarily think that God does not exist, but they feel God’s existence cannot be proven.Atheism, on the other hand is the belief that there are no gods. According to American Atheists, Atheism is not a belief system or religion. They further state that Atheism is not a disbelief in God or a denial of gods, but is a lack of belief in gods and supernatural systems. For many atheists, their beliefs are as strong as those who believe in a particular religion or specific God/gods. Home Health Aides/Personal Care Aides must take care to never judge a person based on their beliefs.
Buddhism
Buddhism is based on the teachings of Siddhartha Gautama, known as Buddha (PBS, 1999). While this religion started in Asia, it is practiced worldwide. According to PBS, Buddhists believe in The Four Noble Truths: that suffering exists, that there is a cause to the suffering, there is an end to the suffering, and there is a way to bring the suffering to an end. Desiring material belongings, immortality, and pleasure leads to suffering. To end suffering, one must achieve Nirvana, which is a state of spiritual heightening in which there are no desires or suffering. To achieve this, Buddhists believe they must follow the Noble Eightfold Path which includes: Right Understanding, Right Thought, Right Speech, Right Action, Right Livelihood, Right Effort, Right Mindfulness, and Right Concentration (PBS). Practicing meditation, good moral conduct, and achieving insight are the ways to follow this path. Death is viewed as the ending of the physical body, and the spirit will live on in a new form, or rebirth occurs. After the death of a person who practices Buddhism, the body should be left alone for 3-8 hours untouched, as the Buddhists believe that the spirit lingers for some time (Carteret, 2010e).
Christianity
Christianity is the world’s largest religion and is based on the teachings of Jesus Christ, who lived 2,000 years ago (BBC, 2011a). Christians believe that Jesus was the Son of God who was sent to Earth to save humans from the consequences of their sins. Important holy days include Easter and Christmas. Christians believe that Jesus gave his life on the cross (Crucifixion), which occurs on Good Friday, and that he rose on the third day (Resurrection), which is Easter day. Christmas marks the day of Jesus’ birth. The Christian holy book is called The Holy Bible, which consists of the Old and the New Testaments. Most Christians worship in a church and communicate with God through prayer. Christians believe in baptism, which is the process in which a formal commitment is made to God (BBC, 2009e). There are many denominations of Christianity, each with a different set of practices. Some of these groups include Methodist, Mormon, Presbyterian, Baptist, Episcopalian, Seventh-day Adventists, Lutheran, and Roman Catholic. Religious leaders may be called priests, pastors, preachers, or deacons, depending on the denomination. Some Christians may practice dietary restrictions, such as not eating meat or fasting during the Lenten season, which is approximately 40 days prior to Easter, starting on Ash Wednesday. Mormon diet prohibits tea, cola, and coffee. Some Christians may have sacred objects in their homes or worn as jewelry, such as images of saints and holy crosses.
Hinduism
Hinduism is largely practiced in India. It is the world’s oldest religion, and there is no founder. There are four sects, or divisions, of Hinduism: Shaivism, Shaktism, Vaishnavism, and Smartism (Kauai’s Hindu Monastery, 2015.). Each has some different beliefs and practices, but all believe in one Supreme Being, who is the creator of all things. According to Kauai’s Hindu Monastery, Hindus follow the four Vedas, which are ancient scriptures. Hindus also believe in reincarnation, which is the belief that the soul reincarnates, or returns after the physical body has died into a new body. This process is meant to help karma become resolved. Karma is the belief that consequences are caused by actions, and that people create their own destinies by their thoughts and actions. Hindus believe that all life is sacred. Many may be vegetarians. After the death of a person who practices Hinduism, the body must be bathed, massaged with oil, dressed, and cremated prior to the next sunrise (Carteret, 2010e).
Islam
Islam, the second largest religion in the world, began in Mecca, Arabia over 1400 years ago (BBC, 2009b). People who practice Islam are called Muslims. Prophets of this religion include Adam, Moses, Abraham, David, Jesus, and the final prophet to whom credit for the start of Islam is given; Muhammad (BBC, 2011d). Muslims believe in one God, called Allah. Many Muslims pray five times per day, facing Mecca, the holy city. Mosques are the places of worship for Muslims. Outside of mosques is a place for people to leave their shoes and to wash prior to entering to pray (BBC, 2009g). Prayer is done sitting on the floor and facing the direction of Mecca. Mostly men attend prayer services in mosques, and when women do, they pray in a section separate from the men. The Qur’an, which is the sacred word of God as revealed to the prophet Muhammad over 23 years is the holy book of the Islamic faith (BBC, 2011c).
Muslims believe in predestination, that Allah has knowledge of all that will happen (BBC, 2011d). However, Muslims do believe in free will, that they can make their own choices in life. Muslims also believe in the Day of Judgment, in which every human will be judged to determine if they will go to heaven or hell (BBC, 2011d). According to BBC (2009i), the most important practices of Muslims are the Five Pillars. These are obligations that every Muslim must meet within their life in order to get to heaven. They include being sincere within one’s Muslim faith, praying five times per day, paying charity to the poor, fasting during Ramadan, and making a pilgrimage (a visit of faith) to Mecca once in their lifetimes (BBC, 2009i). Ramadan, a holy period, is the ninth month in the Islamic calendar (BBC, 2011b). According to BBC (2011b), during this month, adults must give up food and drink, smoking, and sexual activity during daylight hours. The month of Ramadan ends with the festival known as Eid al-Fitr, in which Muhammad is thanked for giving Muslims strength to practice self-control over the last month (BBC, 2011e). Celebrations with family and services are attended at mosques in which Muslims wear new or their best clothing (BBC, 2011e).
There are special rules regarding diet and dress that many Muslims follow. Most Muslims do not consume alcohol or pork. Women dress modestly with long skirts and shirts within the Muslim faith and may wear a hijab, a veil covering the head and chest (BBC, 2009h). Some Muslims believe all parts of a female should be covered except the eyes, while others believe all parts should be covered except the face and hands. The name for the garment which covers all of a woman except her eyes is called a burqa. It may be forbidden for members of the opposite sex to touch. It is important for healthcare workers to be aware of these dietary restrictions and any special way of dressing their patient may practice.
Judaism
Judaism originated in the Middle East over 3500 years ago and was founded by Moses, although Jews trace their history back to Abraham (BBC, 2009a). Abraham was a leader appointed by God and was the first to teach that there was only one God. The Torah, written in Hebrew, which is the oldest Jewish language, is the religious book of the Jews and consists of the 5 books of Moses (BBC, 2009e). According to BBC (2009e), Jewish people believe that God dictated the words found within the Torah to Moses on Mount Sinai, after the Jews were exiled from their slavery in Egypt. Additionally, the Torah is read in completion every year during synagogue or temple, which is where Jewish people attend services (BBC, 2009a). The Torah contains 613 commandments by which Jews live their life (BBC, 2009e). A rabbi usually conducts services within synagogues and temples, and serves as a religious leader for Jewish people.
Judaism is divided into Reform, Conservative, and Orthodox movements, all with some differences in practice and belief. In Orthodox Judaism, men and women sit separately in synagogues and services are conducted in ancient Hebrew. Some Jewish men wear a yarmulke or kippah, a small cap to cover their head. Health care providers should take care to respect religious dress and special traditions their patients may follow during prayers and religious holy days.
The holy day is called the Sabbath, which begins at nightfall on Friday and lasts until nightfall on Saturday (BBC, 2009d). The Sabbath is a time of rest and worship, in which candles may be lit, the Sabbath wine and meals with prayer shared. Hanukkah is the Jewish Festival of Lights, lasting 8 days, in which a menorah with 8 candles is lit, one each day. This holiday celebrates the Jewish people’s struggle for religious freedom (BBC, 2009c). Rosh Hashanah is another holy day which lasts two days, in which the creation of the world is celebrated on this Jewish New Year (BBC, 2011f). According to BBC (2011f), this day is also known as Judgment Day, in which God reviews one’s good versus bad days throughout the year. On Yom Kippur, or Day of Atonement, which is the most sacred day of the year for Jewish people, marks the day when God’s judgment comes to an end (BBC, 2011g). The Book of Life, in which one’s year has been reviewed closes. This determines how the course of the next year will go for each person (BBC, 2011g). During holy days and the Sabbath, special foods are shared and fasting may occur, such as in the 25 hours prior to Yom Kippur (BBC, 2009c; 2009d; 2011g). Healthcare providers should take special care to honor these dietary and fasting practices in order to best uphold their patient’s religious beliefs.
Family & Diversity
Families play an important part in most people’s lives. It is important to keep in mind that what “family” means differs from person to person. There are many different kinds of families. This unit will explore different types of families that healthcare providers may encounter.
What makes up a family?
Nuclear families: Nuclear families include a father, mother, and at least one child. About half of all families are nuclear families (American Academy of Pediatrics, 2015).
Single–parent families: Single-parent families include one parent and one or more children. Approximately 27% of households are made up of single-parent families (American Academy of Pediatrics, 2015).
Same–sex parent families: Same-sex parent families include couples of the same sex (gay, lesbian, or bisexual) with one or more children. Approximately 2 million children in the U.S. have same-sex parents (American Academy of Pediatrics, 2015).
Unmarried couples: In families with unmarried couples, the couples may be the same-sex or opposite-sex and with or without children. About 1.5 million children in the U.S. have parents who have never married (American Academy of Pediatrics, 2015).
Couples without children: Some families include couples who are married or committed to one another, but do not have children. Couples may or may not live together, but consider their unit to be part of what makes up their family.
Extended families: In some families, parents, children, grandparents, aunts, uncles, cousins, other relatives, and even friends may be considered to be part of a patient’s extended family.
Blended families: Blended families consist of divorced or widowed parents who have remarried and have children from previous relationships. They may also have children from the current marriage. About 20% of children in the U.S. live in blended families (American Academy of Pediatrics, 2015).
Grandparents as parents: In some families, one or more grandparent serves as the child/children’s’ parent(s). Approximately 1.3 million children in the U.S. have grandparents who serve as their parent (American Academy of Pediatrics, 2015).
Adoptive/foster families: Some families have adoptive or foster children live. About 120,000 children are adopted each year and 6.3 children out of 1,000 live in foster homes (American Academy of Pediatrics, 2015).
A patient’s family may be different than that of the Home Health Aide/Personal Care Aide. Who they consider family may not be the people who you identify as family. Some people don’t have any living family or their family lives far away. They may rely on neighbors and friends to help them, and consider these people part of their family. Whatever kind of family a patient has, it is important to recognize the important role they have in a patient’s life. Any person within a family may help a patient to make important health-care decisions, provide daily care, drive the person to appointments, contact the health-care team on behalf of the patient, or provide emotional support to the patient. Remember, family is who the patient says is family.
Supporting Family Members
Family members must also adjust to a patient’s illness or disability. They may have trouble accepting the consequences of the illness or disability. Family members have many kinds of reactions to a loved one becoming sick. They may be afraid, sad, angry, or frustrated. There are numerous reasons for this. They may be concerned with finances and how to pay for their family members’ medical expenses and medicines. They may be dealing with the patient not being able to work due to their illness and disability, and are concerned with how to meet the family expenses. They may be confused with the large amount of paperwork that needs to be filled out and trying to understand medical information related to their loved one. Family members may also be physically tired from providing daily care for the patient or from frequently traveling to and from the patient’s home to care for or visit them. They may also be afraid their loved one will never become well, or worse, die. Home Health Aides/Personal Care Aides play an important role in caring for their patient and their family.
Health Aides/Personal Care Aides must be sensitive to the adjustments their patient’s family must make. They should perform their job well and refer any issues that they cannot competently handle to their supervisor. Empathize with family members. This means try to understand how they feel. If a family member comes to them with a problem, listen to their concerns. Sometimes just talking about a problem can make a person feel better about it. Be supportive and encouraging. Try not to use cliché phrases such as, “It will all work out.” Being able to paraphrase (summarize) what the person says and the feelings they are conveying (what they are trying to express) is most helpful.
If a family member or patient says, “I am scared”, or “I am so stressed out”, the Home Health Aide/Personal Care Aide can use reflection to let them know they have heard them and understand how they feel.Phrases such as: “You are feeling scared”, “I can imagine how stressful this must be for you” or “You are feeling anxious about what will happen to (patient name)” lets a person know that you are listening to them. If the problem is out of their ability to handle, they should contact their supervisor for assistance.
Be respectful of family members and allow for privacy during visits. Report to the supervisor any obvious changes or problems with the patient resulting from family visits or involvement. Not every patient has good relationships with their family. For example, if a Home Health Aide/Personal Care Aide notices abusive behavior or language, it is important that they immediately report this to their supervisor. If they notice that their patient becomes depressed or their mood changes, they must document and report these findings to their supervisor immediately. These could be signs of potential abuse.
Unit B: Communication Skills & Developing a Therapeutic Relationship
Communication
“To effectively communicate, we must realize that we are all different in the way we perceive the world and use this understanding as a guide to our communication with others” –Anthony Robbins
Communication is the process of exchanging information with others and is a means for two or more people to connect. Communication is an essential part of the job of a HHA/PCA. They must be able to communicate with their supervisor, members of the healthcare team, the patient, and family members.
Principles of effective communication: The principles (basics) of communication include the following elements:
- Sender: the person who sends the message
- Receiver: the person who receives the message
- Feedback: the receiver responds to the message in some way to let the sender know they heard and understood the message
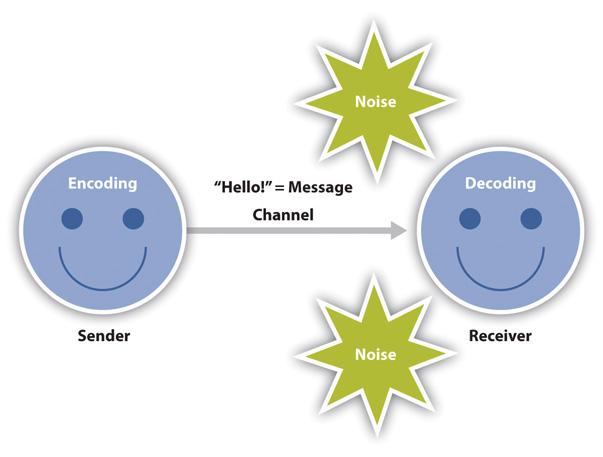
Feedback is very important in communication. It is especially important in the work of a HHA/PCA. They must take the time to ensure that their patients understand the message you are trying to convey. During a communication, there is a repetitive cycle of sending-receiving-feedback between the communicators. During the process of communication, there are two types of important communication: verbal and nonverbal communication.
Verbal communication involves the use of words or sounds, which are either spoken or written. These are the actual spoken words that are said or written during a conversation. Nonverbal communication on the other hand is the way we communicate without using words. Shaking a head, rolling eyes, smiling, or crying are nonverbal methods of communication.
It is important to remember that the receiver of the communication (e.g. the patient) sees the nonverbal communication the sender (e.g. the healthcare worker) demonstrates in addition to hearing the spoken word. There are many aspects of nonverbal communication the Home Health Aide/Personal Care Aide should pay attention to. Tone of voice is an important nonverbal method of communication. The tone of a person’s voice often reflects their mood and can convey a different meaning to a sentence. For example, you might say, “Oh, really?!” with an emphasis on the “Oh!” to convey your surprise. Take the same sentence and emphasize the “really” and it changes the meaning of the sentence to one of disbelief or sarcasm: “Oh, really?” Saying the same sentence with a different tone of voice and emphasizing certain words sends a completely different message. Body language is another form of non-verbal communication. The way we sit or stand with shoulders forward or slouched down, the way we hold our arms either crossed in front of our chest or at our sides all convey a message to the receiver. The way we use gestures, touch, and even silence also tells the receiver what we are thinking and feeling.
Sometimes, people send one message verbally and quite another non-verbally. We can often tell a person‘s true feeling with the nonverbal message they send. For Home Health Aides/Personal Care Aides it is important to be aware of these incongruous messages (where one message contradicts another message). If a patient tells them, “I feel fine,” yet they sigh and are sitting with shoulders slumped down and appear to be crying, this is a good indicator that their verbal and nonverbal messages are incongruent (do not match).Home Health Aides/Personal Care Aides’ ability to be aware of these differences will help them provide the best care possible. When they do notice these confusing messages, they should try to find out if they are correct in their thinking. Say something like, “Mrs. Martin, you say you feel fine but it looks like you have been crying. Are you sad?” This helps to clarify if they have understood the message and can help open up the lines of communication for an important and honest discussion of how Mrs. Martin is really feeling.
It is also important to be aware of the congruence of your own verbal and nonverbal messages. Does your body language match your words? Is your tone of voice upbeat or flat and uninviting? Are you making eye contact with a patient and smiling as you tell them you are glad to see them or are you looking at the floor when you say this rather than their eye? Patients will read into these mixed messages and feel that the HHA/PCA is not really glad to see them or to be taking care of them today.
The use of nonverbal communication varies from culture to culture. In some cultures, touch is an important part of communication. Yet, in other cultures, touching another person, especially if uninvited, is disrespectful. Eye contact is also another form of nonverbal communication that varies among cultures. Some cultures value eye contact while speaking, while other cultures consider eye contact while speaking rude. The proximity or closeness of how two people stand together during a conversation may also vary among cultures and personal preferences. Standing too close to someone during conversation could appear to be a threat to some people, while others value standing close to the person they are conversing with. It is important to get to know the patient and their cultural and personal preferences in order to be respectful of cultural differences. If Home Health Aides/Personal Care Aides are unsure, they should ask their patient to tell them about the values of their culture and follow their lead during conversation. If, for example, they startle when you touch their hand while talking, or pull their hand away from you, this is an indicator the person does not like to be touched while talking. It is always a good idea to make sure a patient knows that you are going to touch them in order to provide care. Permission should always be obtained from the patient.
Self-Check Activity M2-8
1. Which of the following is an example of a nonverbal communication?
a). Saying, “I don’t care.”
b). Shrugging one’s shoulders
2. Which of the following is an example of a nonverbal communication?
a). Calling your dog to come to you
b). Clapping to get your dog’s attention
Barriers to effective communication
Language Barriers
If a patient’s first language is a different language than that of the HHA/PCA, speak slowly and clearly with short and simple messages. Consider using pictures or pointing to objects if it is difficult to explain or for the patient to understand certain words. For instance, if the patient is having trouble understanding when the HHA/PCA asks if he would like to use the bedpan, they could show or point to the bedpan to convey their message. If their patient does not speak their language at all, they should speak to their supervisor about using a translator to assist them and their patient to communicate while they provide care. In some instances, family members may be able to translate for the patient. A word of caution with using family members to translate is that the patient may not be able to tell them what he or she really wants or feels as they may not want to upset their family member if their wishes go against what their family wants.
Hearing Bmpairment
In patients who have a hearing impairment, meaning they have difficulty with hearing or are deaf, the HHA/PCA must be sure to stand directly in front of the patient so that the patient may see them during communication. If they have a hearing aid, check to make sure it is turned on, that the volume is high enough, and that the batteries are in good working order. Speak in a low, clear, and pleasant voice. Be careful not to shout or yell. Higher pitched tones such as yelling are not effective in helping a person hear. Even if the person can’t hear what is being said, they will feel as if they are being yelled at by the body language they see. Be cautious to not become frustrated as a patient will pick up on all nonverbal communication.
Visual Impairment
If a patient has a visual impairment, do not forget that voice is not the only part of the conversation. It is important that they be able to see body language and facial expressions in order to understand the full effects of the message. If a patient wears glasses, be sure they are on and that the lenses are clean. In patients who are legally blind, Home Health Aides/Personal Care Aides should be careful to let them know where they are in relation to them and explain in detail any information that they could not pick up on without seeing. For example, if they are reading to a patient who is legally blind and there is a picture they cannot see, they should explain to the patient the picture in detail so that they can see it with their mind’s eye. When serving meals to a patient who is legally blind, they should place eating utensils where they can reach and tell them where they are in relation to their hands. Use the clock method to let them know where their food is. For example, “Mrs. King, your mashed potatoes are at 6:00.”
Aphasia/Speech Impairment
Sometimes people have speech impairments that make it difficult for them to send messages so that others can understand. Aphasia is a language disorder in which a patient has difficulty understanding or expressing language. People can develop aphasia as a result of a stroke, brain injury, or dementia. Listen very carefully to what a patient is trying to convey. Home Health Aides/Personal Care Aides should ask them for clarification if they are not sure of a word. They should not just nod and agree if they do not understand what they have said. It is just as, and perhaps even more frustrating for them to feel misunderstood or not heard as it is for Home Health Aides/Personal Care Aides to have trouble understanding their patient. In some instances, alternatives to voice may be used as effective means of communication. These can include white boards, chalk boards, and note paper so that the patient may write down what they wish to communicate. Providing these materials to the patient lets them know that the HHA/PCA cares about what they have to say and wants to ensure their needs are met.
Cognitive Impairment
If a patient has a cognitive impairment, meaning that they have difficulty processing (understanding) information, take extra time when explaining something to them. They may need a longer period of time to try to understand the message being sent. Avoid long sentences. Use shorter, simple ones. Allow time for the patient to process what was said before moving on to the next sentence or topic. Check with the patient to make sure they understand. Sometimes people will agree with someone even if they do not understand, as they may be embarrassed or do not want you to become frustrated with them. Remember to be patient and kind. Home Health Aides/Personal Care Aides must watch their tone of voice, facial expression, and body language, as these all convey their true feelings.
Yes/No Questions
Yes and no questions tend to shorten a conversation. For example, if Home Health Aides/Personal Care Aides ask a patient, “Does it hurt?” their response will be either yes or no. If they respond yes, they are still unsure about the meaning and extent of the pain. If instead they ask, “Tell me about your pain,” they are opening the lines of communication for the patient to be descriptive about their pain. This makes it more likely that they will understand how their patient feels and will be able to care for them properly. Asking a patient, “How many children do you have?” results in a shorter conversation versus, “Tell me about your children.” Try to use open–ended questions in order to allow the patient the chance to speak in more depth. Open-ended questions will show the patient that what they have to say is important. Closed–ended questions such as yes/no questions end the conversation quickly and demonstrate to the patient that their thoughts are not important.
Asking “Why?”Questions
Asking “why?” when a patient makes a statement is another way to quickly end a conversation. It also could make the person feel defensive. If a patient does not want to do something, such as take a bath, don’t simply ask, “Why?” Say something instead such as, “You usually enjoy your bath. Tell me how you are feeling today.” The patient may then be more likely to share their thoughts and feelings.
Use of Clichés
Clichés are catch phrases people use repeatedly that do not really mean anything at all. People tend to use clichés when they are unsure of what to say. The use of clichés, especially when someone is trying to convey their feelings is a sure way to end a conversation. Home Health Aides/Personal Care Aides should try to avoid using clichés such as, “Oh, it will be alright,” “Things will get better,” “I know just how you feel,” or “We are never given more than we can handle”. Phrases, or clichés, like these tend to end conversations. They can also make a person feel patronized or as if you are treating them like a child.
Using clichés conveys to the person with whom you are speaking that you do not want to explore their true feelings. You can never guarantee an outcome such as a patient getting better, so be cautious to not say that they will get better. Home Health Aides/Personal Care Aides cannot truly understand how their patient feels as they have not walked in their shoes. Instead, they should try phrases such as, “I understand that this seems scary for you. What can I do to make you feel more comfortable?” or “You seem very anxious right now. Tell me how you are feeling.” This allows their patient the room to explore their thoughts. It also demonstrates that they care about how the patient feels. Be cautious too, with using clichés as they tend to be culturally relevant, meaning they do not have the same meaning from one culture to the next.
Self-Check Activity M2-9
True or False
1. To help improve communication between a HHA/PCA and a patient, ensure eyeglasses are on and hearing aides are in if the patient wears them. ________
2. It is okay to tell a patient, “Things will get better”, “Don’t worry” and “I know how you feel” to help them feel better and to cheer them up. _______
3. Using closed-ended questions such as ‘yes/no’ and ‘why’ questions will help to encourage a patient to express themselves. ________
4. Providing patients with a chalkboard or paper and a pen can be a useful way to help them express themselves if they have trouble with speech. _______
5. It is important to be patient and to watch nonverbal communication cues such as tone of voice and body language when communicating with a person with a speech or cognitive disorder.
Active Listening
“Most people do not listen with the intent to understand; they listen with the intent to reply”–Stephen R. Covey
Active listening means what it sounds like.It means that you are fully concentrating on what is being said, rather than passively listening or focusing on your reply. You are actively paying attention or listening to the other person with whom you are speaking. Active listening is an important skill for a HHA/PCA to develop. It demonstrates to their patients that they care and are interested in them. It also allows them to obtain important information about their patient’s health care needs.
Active listening means giving the speaker, or sender of the message, your full attention. It means using all your senses while listening. Active listening means paying attention to the words the speaker is saying and the nonverbal messages that are also being expressed. Active listening means conveying (showing) the other person that you are interested in what they are saying. We demonstrate active listening by not only our spoken words. Unspoken words or our nonverbal messages also demonstrate that we are actively listening. Nonverbal messages, such as use of eye contact, posture, nodding of the head, touch, and facial expressions like smiling convey the powerful message that we are actively listening to the speaker.
How to Be a Good Listener:
- Allow the person the opportunity to express his/her ideas completely. Concentrate on what they are saying. Do not interrupt. Avoid finishing their sentences, even if you are in a hurry, if you think you know what they are going to say, if they have told you the same thing before, or if they are having trouble communicating and are taking a long time to respond. If you find it particularly difficult to not interrupt, practice counting to ten when you feel the urge to interrupt.
- Restate the message you heard the other person saying to ensure you heard them correctly. This feedback allows the other person to correct any misunderstandings and demonstrates you were listening to and heard them. For instance, you can something like, “I heard you saying that you are not happy with your new diet.”
- Provide feedback while you are listening to encourage the person to continue and show you are interested. Leading statements such as, “Go on,” “Mmm–hmm,” “Yes,” and “Tell me more,” encourages the person to continue and demonstrates your interest in what they have to say. Use of body language such as nodding your head helps to encourage the person to continue.
- Allow for silence. Silence can be a powerful tool. Silence allows the person a chance to fully explore and express their thoughts. Often, we try to avoid silence because it makes us uncomfortable. Silence is especially important when discussing sensitive or difficult topics. Don’t rush to fill in the silence with meaningless conversation or clichés.
- Avoid changing the subject even if the topic makes you uncomfortable. This conveys to the patient that you are not interested in what they are saying. For example, a patient might say, “I am really afraid to die,” do not say something like, “Don‘t think like that. Come on, let‘s do something to cheer you up.” Instead say something like, “You are afraid you are going to die. Tell me what‘s on your mind.”
- Use your body language to demonstrate your interest in the other person. Stop other tasks you are doing and put your full attention on the person in front of you. Stand, or better yet, sit, facing them. If appropriate for the culture, make eye contact. If a patient enjoys touch as a means of communication, a HHA/PCA can touch their hand or arm while they are talking. Use facial expressions to convey your interest and attention. Smile as appropriate and appear concerned when a difficult topic is being discussed. Lean forward to convey your interest and avoid crossing your arms over your chest, which closes you off from the other person.
- Be aware of cultural differences. Get to know a patient’s culture and what is acceptable. Learn the words and expressions of a patient’s culture to fully understand the message they are trying to convey. When in doubt, ask a patient to explain what a phrase or expression means. Do not assume you understand.
- Do not talk to an elderly or disabled person as if they are a child. Talk to them as if you would anyone else. Do not call them names such as “Honey,” “Sweetheart,” or “Dear.” Call the person by the name they wish to be called. Always ask how the person would like to be referred. Some people may find it inappropriate if you call them by their first name. They may prefer to be addressed as “Mr.” or “Mrs.”
- Avoid fidgeting during conversation. Do not look at the clock while people are speaking as this conveys that you are in a hurry or bored. Avoid picking at your fingernails or clothing, playing with your hair, doodling, or using your cell phone while the person is speaking. Home Health Aides/Personal Care Aides should give their patient their full attention.
- Use empathy. Try to put yourself in another person’s shoes to understand what they are going through. Don’t state, “I understand how you feel” as you cannot know exactly how they feel.
- Ensure communication aides such as hearing aids, eyeglasses, and dentures are clean and in good working order. Home Health Aides/Personal Care Aides should provide them to their patient to help them communicate more effectively.
Self-Check Activity m2-10
Self-Check M2-10
Which of these two scenarios demonstrates active listening?
1. Mrs. Pompi is in her bed and is telling her HHA that she is scared she will never walk again. The HHA is cleaning the room as Mrs. Pompi talks and periodically says, “Mhmmm” and “Okay” during the conversation. The HHA is worried that she will not get all her tasks completed before she has to leave for the day. She looks at the clock on the wall every now and then as she works and Mrs. Pompi talks. Mrs. Pompi says, “I just don’t want to live the rest of my life in this bed. I’m so scared.” The HHA says to her, “Don’t worry about that, honey.I understand how you feel. Everything will be okay. Now, let’s get you washed and dressed.”
2. Mrs. Williams is in her wheelchair doing a crossword puzzle while the HHA makes her bed. Suddenly she looks up from her crossword and says, “I am so frightened that I am going to die. I don’t want to die yet.” The HHA stops what she is doing, pulls a chair next to Mrs. Williams and touches her hand. The HHA says, “You sound scared and worried about dying. Would you like to talk about it?”
Therapeutic Relationship
A therapeutic relationship means creating a positive alliance, or relationship, with a patient. Establishing a therapeutic relationship with a patient takes time, practice, and skill. It is important for a HHA/PCA to take the time to establish a good working relationship with their patient. It will make all the difference in their ability to provide good care to their patient and for their patient to feel good about the care they receive.
The relationship between a HHA/PCA and their patient/family is different from the one they have with their own family or friends. The relationship the HHA/PCA has with their own family and friends is reciprocal, or mutual, meaning both they and their family member share goals and work to meet each other’s needs. The relationship they have with their patients and their families is one where they focus on their patient’s needs, problems, and goals. While they may take on many roles with their patients and the patients may come to view the HHA/PCA as “family,” or as a “friend”, it is important to always remember that Home Health Aides/Personal Care Aides are there to care for the patient. The patients cannot work to help the HHA/PCA meet their own needs. This does not mean that Home Health Aides/Personal Care Aides are not friendly with their patients and their families. It just means that they must always focus on their patient and be aware of professional boundaries.
How to Establish a Therapeutic Relationship:
- Trust: Especially during the first few interactions with a patient and their family, it is important for Home Health Aides/Personal Care Aides to demonstrate that they are trustworthy. This means showing up when they say they will, performing tasks and skills well, being honest, and demonstrating their concern for their patient’s well-being.
- Setting boundaries: When meeting a patient and their family, Home Health Aides/Personal Care Aides should let them know who they are and what their role is. Tell them the tasks they can and cannot perform. For instance, they can say something like, “I am Karen. I will be your HHA/PCA. If it is okay with you, I will be coming here Monday, Wednesday, and Friday to help you bathe, dress, and eat. I am also here to be a support to you and your family.” If a patient/family asks a HHA/PCA to perform a task they are either not trained to do, is outside of their scope of practice, or that they are uncomfortable with, let them know, and inform their supervisor. They can say something to the effect of, “I‘m sorry, I am not able to put a catheter in you. I will let your nurse know that this is something you need help with.”
- Confidentiality: It is important to let their patients know that they will protect their privacy. However, they should never tell a patient that they will keep something a secret, especially from their supervisor and the rest of the healthcare team. If a patient asks if they can tell their HHA/PCA a secret and that they not tell their nurse, they should politely let them know they cannot do this as their whole team is there to help care for them. They can say something like, “Mr. Thorpe, I cannot keep a secret from your nurse or doctor. They are here to help care for you. I do have to share what we do and talk about with my supervisor so that she knows you are properly being cared for. However, I will not share what you tell me with anyone outside of your health–care team if you do not wish.”
- Empathy: Having empathy for another person means that you understand the thoughts and feelings of the other person. Empathy is different from sympathy. With sympathy, we feel sorry for another person. Home Health Aides/Personal Care Aides should be careful not to feel sorry for their patient as this often comes across as pity, or being condescending (looking down upon a person), which most people do not like. Sympathy is also more of an expression of one’s own feelings, while empathy shows one understands a patient‘s feelings. In expressing sympathy, we are showing agreement with the other person instead of helping them explore their feelings. Demonstrating that they are empathetic, or understanding, of their patient’s thoughts and feelings shows their patient that they care for them and are there to help them.
Examples
Scenario: Here is an example of the difference between sympathy and empathy. In this scenario a patient has just told their HHA/PCA that they have been diagnosed with cancer.
- Sympathetic response: “Oh! I am so sorry! That is terrible! I know exactly how you feel. My mother was diagnosed with cancer last year and it has been just awful.” You then go on to describe the situation with your mom and how upsetting it has been to deal with her diagnosis.
- Empathetic response: “How upsetting this must be for you. When my mom was diagnosed with cancer last year I had so many different emotions. What are your thoughts and feelings about your diagnosis?” You then sit with the patient and allow them the time and space to explore their thoughts and feelings. Here, the focus is on the patient and not on you.
- Positive regard: Positive regard is respecting another person and demonstrating that you value them as a person, regardless of your differences, and whether or not you agree with their thoughts, feelings, or behaviors. We demonstrate our positive regard for someone by our verbal and nonverbal communication. What we say, how we say it, and our body language all demonstrate our respect for another person. If a patient does something that the HHA/PCA does not approve of or says something that is in disagreement with their own beliefs, it is important for them to convey to the patient that they are not judging them. Home Health Aides/Personal Care Aides should watch their tone of voice, facial expressions, and body language. For example, a patient may tell a HHA/PCA that they have decided to stop receiving life-saving treatments. While they may not agree with their decision, they must convey an understanding of and respect for their decision. “Mr. Wahlman, that must have been a difficult decision for you to make. How are you feeling about it?” This response demonstrates that they respect their right to make a decision and are interested in understanding how they feel about it.
Setting Boundaries
It is important as a HHA/PCA that boundaries are set in order to best meet the needs of the patient. According to the National Council of State Boards of Nursing (2014), certain “red flag” behaviors can indicate boundaries are being blurred. These can include: discussing personal issues with a patient, keeping secrets with or for a patient, flirting with a patient, gossiping or “bad-mouthing” co-workers and others on the treatment team, spending more time than necessary with a patient, believing you are the only one who understands or can provide proper care for the patient, showing favoritism toward a patient, and meeting with a patient or their family outside of the designated treatment areas.
Behaviors such as over-helping, controlling, and possessiveness over the patient can indicate that boundaries have become blurred. When relationships are terminated, intense emotions may arise leading the health care worker to engage in behaviors such as continuing to visit the patient, which are unprofessional and unhealthy for the patient. These are important issues to consider in order to set and maintain appropriate professional boundaries with patients.
- Over–helping: Sometimes, we want to help others so much that we take away their independence. For HHAs/PCAs, it is important that they properly care for their patient and help them with what they cannot do for themselves. It is also equally important that they work to promote their independence so the patients do not become too reliant on the HHA/PCA and not do for themselves what they are capable. Promoting independence helps to boost a person’s self-esteem and helps to avoid feelings of helplessness and worthlessness. For instance a patient who is capable of cutting their food might say, “Can you cut this for me? I am too tired.” The response can be something like, “I understand that you are feeling tired today, but it is important that you do things for yourself that you are able. One of the goals we are working on together is to help you become independent and regain your strength. I will sit with you while you cut your food.” This reminds the patient of the established goals, provides encouragement for them, and demonstrates belief in their capabilities. It also demonstrates that the HHA/PCA will be there for them even when they must complete difficult or tiresome tasks.
- Controlling: At times it may seem easier to “take over” with a patient. Home Health Aides/Personal Care Aides may feel that doing something a certain way is best and that they know what is for the patient’s “own good”.Avoid being too controlling or authoritative (bossy) with patients. Instead of telling them what to do, help them to come to their own decisions by exploring their options. Give patients choices whenever possible. For instance, a HHA/PCA knows that their tasks for the day are to bathe their patient and walk them around their living room. While they may want to do a particular task before the other, give the patient a choice. “I am here to help you bathe and take a walk today. Which one would you like to do first?” Give patients options when meal planning rather than just deciding what food is best for them and that they should eat a certain food for their “own good.” For example, a HHA/PCA could ask, “Would you like a turkey sandwich, meatloaf, or pasta for lunch today?” or “What kind of vegetable would you like with your dinner?”
- Possessiveness: As Home Health Aides/Personal Care Aides develop strong working relationships with their patients and their families, they will come to know them very well. They may come to know them better than other members of the healthcare team. Sometimes, this can lead to feelings of possessiveness over the patient/family. They may feel that they know how to best treat their patient. This leads to a breakdown in the care of the patient among members of the healthcare team. It is important to be aware of these types of feelings.
Examples
Examples of feelings, thoughts, and behaviors that may indicate possessiveness over a patient include:
- Feeling angry toward other health-care team members when they make decisions that the HHA/PCA does not agree with
- Arriving to work early and leaving late to spend extra time with the patient
- Withholding information from other members of the health-care team
- Excessively disclosing personal information about yourself to the patient/family to form a close relationship
- Creating a “you and me against the world” attitude where the HHA/PCA views the patient as more than a patient and sides with their position regardless of the situation.
These types of feelings, thoughts, and behaviors are unhealthy for both the HHA/PCA and the patient. They only serve to create disconnection in the patient’s care and make the patient too reliant on the HHA/PCA. If a HHA/PCA finds that they are starting to become too possessive of their patient, they should speak with their supervisor about their feelings and how to work these out.
- Terminating the relationship: Different from your relationship with your own family or friends, there may be an end date to the relationship between a HHA/PCA and their patient and family. Some patients/families may want to continue to have a relationship with the HHA/PCA. They may ask them to call and visit. Ending a relationship with someone is often very difficult. It can awaken strong feelings in the patient and in the HHA/PCA. Patients may feel uncared for, angry, or depressed that they will no longer be working with the HHA/PCA. It is important for a HHA/PCA to remember to keep professional boundaries while also explaining to the patient how much they have enjoyed and have come to value the relationship you have with them. For example, a patient might say, “Will you come visit me even after you stop working here?” The HHA/PCA can say something like, “I have enjoyed working with you so much. I am not able to continue to come visit you once we have stopped working together. It is against my company‘s policy. Let‘s talk about how you feel about ending our relationship.”
Ending a relationship with their patient may also stir up strong feelings for them. It is important for a HHA/PCA to discuss their feelings and how to handle them with their supervisor and not their patient. They must remember that they are there to care for the patient, not the other way around. The company may have specific policies about termination of relationships. This is an important issue to discuss with a supervisor.
It can be difficult to decide if a behavior is crossing the lines of professional boundaries. A helpful way to decide whether one should proceed with a behavior or not is to follow the following decision tree.
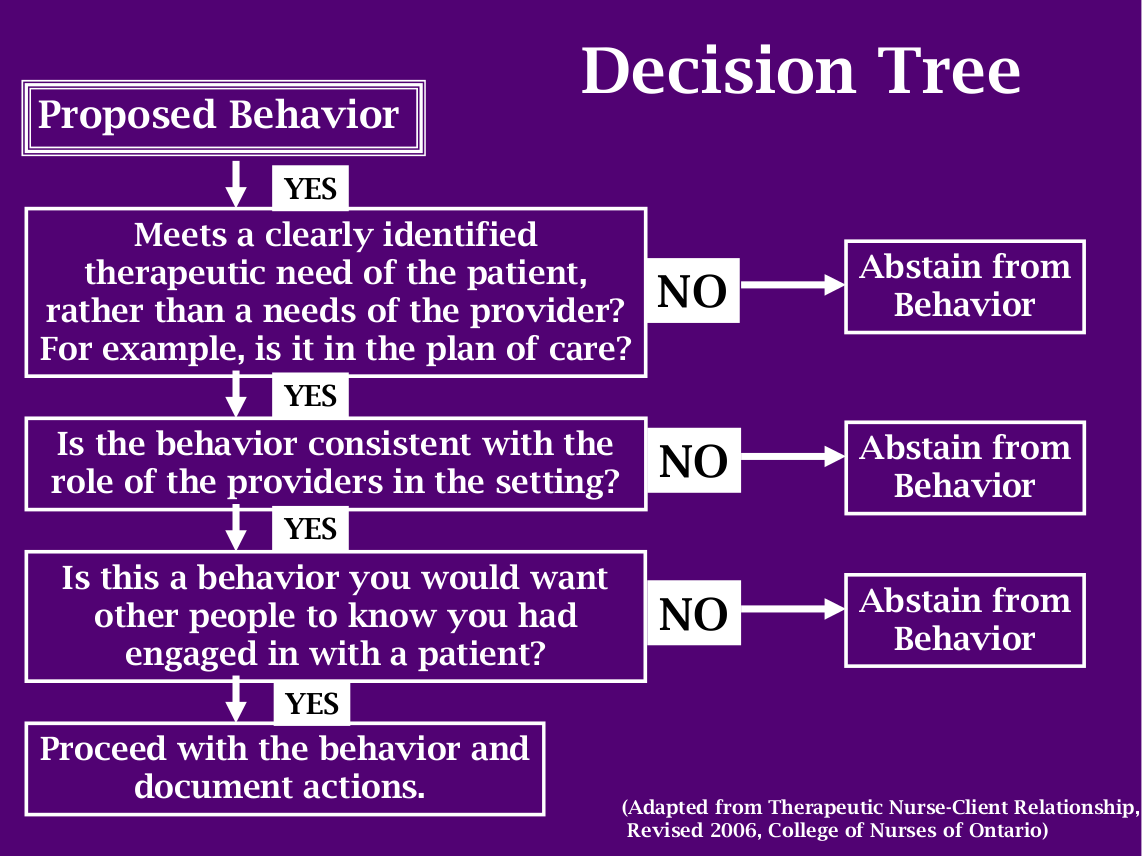
REMEMBER: If a Home Health Aide/Personal Care Aide comes to the realization that the behavior is not part of the care plan, and is not in the best interests of the patient/family, they should not engage in the behavior. If they realize that the behavior is outside of their scope of practice and not within their defined role as a Home Health Aide/Personal Care Aide, they should refrain from the behavior. If they realize that the behavior is not something they would want others to know that they did, they should refrain from the behavior.
Self–check for boundaries: The following is a list of helpful questions the HHA/PCA can ask themselves when determining whether a behavior is crossing a boundary. This list is adapted from Jane W. Barton’s Professional Boundaries: Discerning the Line in the Sand, which can be found at http://www.capnm.ca/Prof_Boundaries_Packet_2010.pdf
- Is this behavior or action in my patient’s best interests?
- Whose needs are being served by engaging in this behavior? Mine or the patient’s?
- Are my actions meant to best meet the needs of my patient or am I meeting my own needs?
- What emotions of my own are being stirred up by this patient/family and are these emotions affecting my ability to effectively make decisions and care for my patient?
- Am I treating this patient differently than other patients with whom I work?
- Will this behavior have an impact on the care I give my patient?
- How would others (healthcare team members, patient’s family) view this behavior?
- Am I taking advantage of the patient?
- Am I comfortable documenting this decision or behavior in the patient’s file?
- Does this decision or behavior go against my agency’s policies?
Self-Check Activity m2-11
Self-Check M2-11
Which of the following would be considered a boundary violation? Answer Yes or No.
- Preparing a pureed diet by following instructions listed in the care plan. ______
- Staying one hour longer past the shift to visit with the patient, making you late for the next home health care patient. ______
- Taking a ten dollar tip from the patient’s family. ______
- Agreeing to continue to visit the patient even after their case has been closed by the agency and they are no longer receiving home health care services. ______
- Providing a bed bath for a patient who requires one daily. ______
- Visiting a patient when you are not scheduled to work. ______
- Turning and positioning a bed bound patient every two hours. ______
- Informing a supervisor about a suspicion about abuse. ______
- Cooking lunch for yourself using the patient’s food. ______
- Not informing a supervisor about a patient’s statement of wanting to die because the HHA/PCA told their patient they would keep it a secret. ______
Documentation
Observing, Recording, Reporting
Recording and reporting information about a patient is an important part of the job of a Home Health Aide/Personal Care Aide. It is important that they understand the types of information that should be included in reports. Information included in reports should always be based on facts.
Objective information is based on information that a person can actually see, hear, touch, or smell (Leahy, Fuzy & Grafe, 2013). It includes actions performed, care provided, and measurements such as how much food or fluid a patient took in or how much urine the patient voided. These types of information are based on fact. Subjective information is information which a person did not see, hear, touch, or smell. It includes statements that a patient has made to a HHA/PCA about how they feel or what they think (Leahy, Fuzy & Grafe).. When recording subjective statements, the HHA/PCA should try to include what the patient stated to them using direct quotes.
Self-Check M2-12
Determine whether the information is objective or subjective
1. The patient states, “My pain is worse than it was this morning.” ____________
2. A HHA/PCA notices that their patient’s right leg is more swollen today than yesterday. ______________
Use of Your Senses
Home Health Aides/Personal Care Aides use all their senses to make observations about their patients and their conditions. Their report includes observations they made by using their senses: sight, hearing, touch, and smell (Leahy, Fuzy & Grafe, 2013).
Sight
The use of sight includes observations Home Health Aides/Personal Care Aides made using their vision. They will note their patient’s condition as they work with them. Changes in appearance, skin, swelling of the legs, weakness while ambulating, new bruises or rashes, trembling of the hands while using a fork and facial expressions are observations they make about their patient using their vision. They may also notice things in the home such as a lack of food or clean clothing for the patient. These are all observations they make through using their sense of sight.
Hearing
The use of hearing is an important sense in a Home Health Aide/Personal Care Assistant’s work with their patient. They will be listening to their patient as they converse. They may notice changes in their patient’s tone of voice, ability to use speech, rate of respiration (breathing), coughing, or gasping for breath.They may hear a patient sighing often to indicate they are tired or sad. These are all observations made through use of their hearing.
Touch
The use of touch is one Home Health Aides/Personal Care Aides will use all the time as they provide hands on care for their patient. They may notice the temperature of their patient’s skin (hot or cold), or feel for moisture if their patient has spilled a cup of water or is sweating. They will use their sense of touch when testing bath water or a bottle for feeding a baby. Their sense of touch will tell them if there are rough edges on their patient’s nails indicating they need to be filed, or wrinkles or moisture on their patient’s linen, indicating they need to be changed. The use of touch allows them to make observations about their patient’s health and helps them to properly care for their patient.
Smell
The use of smell can give Home Health Aides/Personal Care Aides an indicator of the patient’s health and how well they are being cared for. They may notice odors in the home coming from trash that has not been removed, soiled incontinence briefs or urine on bed linens. They may notice an odor from the patient’s body or mouth, indicating they are in need of bathing or mouth care. They may smell alcohol or tobacco coming from their patient or those around their patient. When preparing food, they may notice foul food odors which could indicate that the food has spoiled. Using their nose and sense of smell gives them good information to include in their reports to their supervisor.
What Information to Include in Documentation
The information that Home Health Aides/Personal Care Aides include in their verbal or written report should be of importance and pertinent to the situation. They should avoid including things such as their own personal thoughts about the patient. They should avoid including personal opinions about the patient or their health. For example, they should not write, “I think the patient’s heart failure is worse because she is more short of breath than usual.” They would only record, “Patient reports an increase in shortness of breath. The patient was observed to be short of breath while eating her dinner.” they also want to be careful to not use judgmental statements such as, “Mrs. Smith was very rude to me today.” They do not need to include every detail about the patient or about their visit. For example, it is not necessary to state that they spoke about a favorite television show or that their patient ate soup for lunch (unless the care plan directs them to include specifically what the patient ate). In most instances, they only need to state a percentage of what the patient ate.
Documentation is an important part of their job as a Home Health Aide/Personal Care Aide. It is important to maintain current and timely documentation of tasks they completed and the patient’s condition. It is the way that all members of the healthcare team communicate and become aware of potential problems or changes in the patient’s condition. Documentation protects them and the agency for which they work against liability. A patient’s record is a legal document that can be used in a court of law (Leahy, Fuzy & Grafe, 2013). It is also a necessity to have accurate and timely documentation for insurance and billing purposes.
Document Immediately After the Visit
Home Health Aides/Personal Care Aides should document tasks completed and observations made about their patients immediately after their visit (Leahy, Fuzy & Grafe, 2013).. It is difficult to keep track of so many observations and tasks they completed the longer they wait to document. They may see more than one patient per day. If they document immediately after their visit, they will have better accuracy of information.
If It Is Not Documented, It Did Not Happen
Home Health Aides/Personal Care Aides should also know that if something was not documented, for legal purposes, it did not happen. If they cared for a patient for two hours but forgot to document that they did so, for purposes of the patient chart, they never cared for them that day. Never document care prior to actually providing it (Leahy, Fuzy & Grafe, 2013). This is known as falsifying documents.
Fixing Errors
Use black ink or a computer to type their visit record, depending on their employer’s requirements. If an error is made, never use white out to remove the error. Draw a single line through it and put initials and date next to the error. Then, write in the correct information.
Use Full Name/Title
When documentation is complete, Home Health Aides/Personal Care Aides should sign it with their full name and title.
Dating/Timing Documents
All documentation should be dated and timed. Depending on the agency, regular or military time may be used. If regular time is used, it should be indicated whether the time is AM or PM. For military time, the time is expressed as 0000 hours. From 12 midnight until 12 noon, the time is the same as it is when using regular time, except the 0000 format is used. For example, for 1:00 AM, the time is expressed as 0100 hours. After 1 pm until 11:59 pm, 12 is added to the regular time. For example, if it is 5:00 pm, add 5+12=17. The time would be expressed as 1700 hours. For 9:00 pm, add 9+12=21. The time is expressed as 2100 hours. To change from military time to standard time, you subtract 12. For example, if it was 2330, you would subtract 12. Standard time would be expressed as 11:30.
24-Hour Conversion Table
| Standard Clock (12-Hour Clock) | 24-Hour Clock Conversion |
| 12:00 midnight | 0000 |
| 1:00 am | 0100 |
| 2:00 am | 0200 |
| 3:00 am | 0300 |
| 4:00 am | 0400 |
| 5:00 am | 0500 |
| 6:00 am | 0600 |
| 7:00 am | 0700 |
| 8:00 am | 0800 |
| 9:00 am | 0900 |
| 10:00 am | 1000 |
| 11:00 am | 1100 |
| 12:00 noon | 1200 |
| 1:00 pm | 1300 |
| 2:00 pm | 1400 |
| 3:00 pm | 1500 |
| 4:00 pm | 1600 |
| 5:00 pm | 1700 |
| 6:00 pm | 1800 |
| 7:00 pm | 1900 |
| 8:00 pm | 2000 |
| 9:00 pm | 2100 |
| 10:00 pm | 2200 |
| 11:00 pm | 2300 |
Self-Check Activity M2-13
Convert the 12-hour time to the 24-hour time
1. 1 pm= _______
2. 6 pm=_______
3. 11:30 pm=________
4. 3:30 am=_________
5. 12:00 am=________
Convert the 24-hour time to the 12-hour time.
6. 2200= _________
7. 1930= _________
8. 1815= _________
9. 2330= _________
10. 1300= ________
Confidentiality
Remember to always keep all information in the patient’s chart confidential. It is illegal to disclose information in the patient’s chart without their consent. their employer will provide them with specific training and information about the types of information they will require them to include in their site visit report.
Sample Documentation
Date: 10/30/2014
0900 Assisted with feeding
0930 Provided bed bath, oral care
1000 Assisted with dressing
1015 Changed bed linens, cleaned bedroom
__1.5 hours____ Jennifer Noble, HHA
Total visit time Signature & Title
Self-Check Activity M2-14
True or False
1. It is ok to use white out if you make a mistake documenting. ______
2. All documentation should end with a signed name, title, and include the date and time. ______
3. It is ok for a HHA/PCA to document that they gave the patient a bed bath before they actually did it. ______
4. It is a good idea to document a patient visit immediately after it is completed, before you moving on to the next patient. ______
5. Home Health Aides/Personal Care Aides should include subjective and objective information about the patient’s condition in their documentation, but never judgmental statements or personal opinions. ______
Communicating on the Telephone
Home Health Aides/Personal Care Aides will often use the telephone to communicate with their supervisor and other health care team members. Before making a call, they should plan out what they need to say and if they have a question, think about how they want to ask it. This will help them to keep their phone call to the point to avoid wasting time. It will also help to keep them focused on the purpose of their call. They will also be less likely to forget details that they may have wanted to include during the phone conversation.
When making a call, Home Health Aides/Personal Care Aides should identify themselves and then ask to speak to the person whom they are calling. If the person they need to speak with is unavailable, Home Health Aides/Personal Care Aides should leave a brief message with their name, the phone number where and until what time they can be reached. Do not leave a very detailed message. Leave only as much information as is necessary so that the person knows what they are calling about. Do not leave detailed confidential medical/health information on a message.
Sample phone call (adapted from Leahy, Fuzy & Grafe, 2013)
–Hello, Ms. Lopez, this is Anna Price. I am calling from Mr. Davis’s house. His daughter has a question about whether or not he can have tomato juice on his low sodium diet.
–Ok, so he can have tomato juice if it is the low sodium kind?
–Ok, I will let Mr. Davis’s daughter know this. I will write in my visit notes that you told me to tell Mr. Davis’s daughter that he can have tomato juice if it is labeled low sodium.
–Thank you for your help Ms. Lopez. Goodbye.
Sample phone message (adapted from Leahy, Fuzy & Grafe, 2013)
–Hello, Mrs. Mason , this is Karen Smith. I am a home health aide working with Mr. Chin. The telephone number here is 764-5297. I can be reached at that number until 2:00 pm.
–I am calling because Mr. Chin has a question about his breathing treatments. He would like to know how many times a day he can use his inhaler.
–Thank you very much. Goodbye.
Unit C: Patient Rights
Patient Rights
Patients have the right to receive care that is respectful, compassionate, competent, and that protects their dignity and privacy. Patients have a right to live and be cared for in a safe environment. In addition to keeping a patient’s environment clean and hazard free, providing for a safe environment means that patients are not abused or neglected. Abuse means causing harm to another person. There are many forms of abuse.
Physical Abuse
Physical abuse is any harm, whether unintentional or intentional in which a patient’s body is harmed. This includes slapping, punching, kicking, biting, cutting, bruising, burning, spitting at, pushing, shoving, restraining a person, or handling a person in a rough manner. Physical abuse includes forcing a patient to do something they do not want, such as eat or bathe.
Emotional Abuse
Emotional abuse is abuse that occurs through emotionally causing harm to a person. This includes name calling, yelling at, humiliating, threatening, intimidating, insulting, making fun of a person, treating a person like a child or as if they are unable to think or make their own decisions. Threatening a person in order to make them do something or to not tell on you for something you did or for threatening the patient is also considered emotional abuse. Threatening to take away a patient’s belongings, time spent engaging in pleasurable activities, or to isolate a patient (such as put them in a locked room alone) are all considered emotional abuse.
Financial Abuse
Financial abuse is abuse that occurs with regard to a patient’s finances. This includes stealing money or property, improperly using a person’s money for things other than the intended purpose, taking advantage of a person’s finances, and threatening to cause physical/emotional harm if a person does not give a person their money.
Sexual Abuse
Sexual abuse is abuse that occurs when a person is touched in a way in which they do not wish to be touched. This includes fondling, unwanted touching, and any unwanted sexual activity. Sexual abuse also includes exposing oneself to a person and showing someone pornographic materials that they do not wish to see, or taking pornographic pictures of a person without their consent.
Domestic Violence
Domestic violence is abuse that occurs by spouses, intimate partners, or family members. It can include any type of abuse discussed above, such as physical abuse, emotional abuse, financial abuse, or sexual abuse.
Neglect
Neglect is when a person is harmed by a caregiver, (whether it is a family member or a healthcare worker), when the caregiver fails to provide necessary care. This includes failing to clean a patient up who is soiled, failing to bathe a patient, failing to provide food or fluids to a patient, and failing to turn and position a bedridden patient. Neglect can be just as harmful as abuse. Remember, a patient depends on their HHA/PCA to provide them with the care they need to live.
Home Health Aides/Personal Care Aides must NEVER abuse or neglect a patient in any way. they must also work to protect their patient from abuse/neglect by others, and report ANY suspected abuse/neglect immediately to their supervisor.
Signs of Abuse and Neglect to Report:
- New or unexplained bruises
- Marks that look like they were made from belt straps, buckles, objects, or teeth
- Burns that are unexplained or that are in unusual shapes or places
- Bruises, bleeding, discharge, pain, or swelling in the genital area
- Fractures, dislocated bones, new limping or inability to put weight on a leg or use an arm
- Pressure ulcers and skin tears
- Unexplained mood changes, especially during or after visits from family
- Clothing that does not fit, is torn, dirty, or inappropriate for the weather
- Unsafe and unclean living conditions
- Weight loss, poor appetite, or if the patient appears to be hungry and not well fed
- Bedding and incontinence briefs that are always soiled and appear to have not been changed in a long while
- Rashes, pain, redness in the perineal area (area between the genitals and anus) from lack of cleaning the patient after they have voided
- Violence in the home that a HHA/PCA witnesses including physical or emotional abuse
- Comments made by the patient that indicate abuse or neglect, including reports of family members stealing or using the patient’s money inappropriately
Remember, Home Health Aides/Personal Care Aides are legally responsible for reporting any suspected abuse/neglect. Failure to report suspected abuse/neglect, or actually engaging in any type of abuse/neglect can result in legal and criminal action against a Home Health Aide/Personal Care Aide.
They should document their observations of abuse and contact their supervisor to report their findings. They must use their senses-what did they hear, see, smell or touch that indicates abuse may be or is occurring? They should not be judgmental in their reporting and should not try to interpret what they think is going on.
If abuse is suspected or observed, a report is made by making a phone call to a local Child Protective Services or Adult Protective Services agency. When making the report, Home Health Aides/Personal Care Aides will be asked for specific information about their observations. Remain calm and report only the facts. They may also be asked to provide a written report. their agency will provide them with specific training and guidelines for reporting abuse.
Self-Check M2-15
Which of the following are signs of abuse or neglect?
- Bite marks
- Unexplained bruises
- A family member stealing a patient’s jewelry
- Allowing a patient to lie in their feces and urine for several hours
- Threatening to take away a patient’s treasured necklace if they do not get up to bathe.
- Pushing a forkful of food into a patient’s mouth harshly when they refuse to open their mouth.
- Yelling at the patient in a loud voice
- Telling the patient they are lazy when they refuse to get out of bed
- Not pureeing food for a patient who cannot chew and who is on a pureed diet so that they cannot safely eat
- A new pressure sore appears on Monday after the patient’s caregiver was supposed to take care of the patient over the weekend
The American Hospital Association developed a Patient Bill of Rights, which should be provided by the agency to every person in their care. Patients also have a right to have the Patient Bill of Rights explained to them, and a copy provided to them in a language they understand.
Patient Bill of Rights
(Adapted from the American Hospital Association, 1992).
Remember, the patient is the most important member of the health care team. They have rights that all members of the health care team must respect and uphold.
- The patient has the right to considerate and respectful care.
- The patient has the right to obtain understandable information about their diagnosis, treatment, and prognosis. They have a right to be informed about the risks and benefits of all services and treatments received. Patients also have a right to know the identity (name, license, and health care provider role) of all people involved in their care (doctors, nurses, home health aides/personal care aides).
- The patient has a right to make decisions about the plan of care before receiving treatment. The patient also has the right to refuse any treatment, and to be informed about the medical consequences of refusing treatment. If the patient refuses a specific treatment or care, they still have the right to receive other care services, or to be provided with referrals to services outside of the agency or organization. The patient has the right to participate in the planning of their healthcare and to be informed of any changes in the plan of care prior to the change being made.
- The patient has the right to have an advanced directive or to designate a health care proxy to make decisions for them if they are unable to do so themselves.
- The patient has a right to privacy.
- The patient has a right to expect that all communications and records pertaining to their health and health care will be kept confidential by their healthcare providers, except in cases of suspected abuse and public health hazards when reporting is permitted or required by law.
- The patient has a right to review their health care records and to have the information explained, except when restricted by law.
- The patient has a right to expect that within its capabilities an agency will make reasonable responses to a patient’s requests for medically indicated care and services. If an organization is unable to accommodate such requests, the patient has the right to transfer to another organization which may be able to provide such requests.
- The patient has the right to ask and be informed of any business or financial relationships that exist within the organization which may influence their care.
- The patient has the right to consent or decline participation in research studies, and to be provided with a full explanation about participation in such studies.
- The patient has the right to receive continuity of care and to be informed when such care cannot be provided.
- The patient has the right to be informed of policies and procedures that relate to their care. The patient has the right to be informed of the method they should use to resolve any discrepancies, conflicts, or grievances they may have. They have the right to know the procedure for making complaints if they feel they have not been given the care they deserve. The patient has the right to make complaints without fear of discrimination or negative repercussions for doing so. The patient also has the right to be informed of any charges for services and available payment methods and insurances accepted. This includes being made aware of services not covered by Medicare and Medicaid, and what charges they may be liable for.
Patient Responsibilities
(Adapted from the American Hospital Association, 1992)
As the most important partner in the healthcare team, the patient also has certain responsibilities.
- The patient is responsible for providing information about their health, hospitalizations, and medications, changes in symptoms or health condition. Patients should ask questions and ask for additional information about their health and treatment.
- The patient is responsible to inform their health care provider about their advanced directives and health care proxy and to provide them with a written copy. They are responsible for informing the health care provider about any changes they may make to their advanced directives or healthcare proxy.
- The patient is responsible to inform their health care providers if they expect problems with the treatment and services they are to receive. This includes informing the provider if home visits need to be changed.
- The patient is responsible for being aware of the organization’s policies and procedures and to make reasonable accommodations to meet the needs of the organization.
- The patient is responsible for providing necessary insurance and financial information to the organization in order that payment may be made for services rendered, and to make payment arrangements as necessary.
- The patient is responsible for informing the health care provider of any dissatisfaction with their services.
- The patient is responsible for carrying out mutually agreed upon responsibilities.
- The patient is responsible for providing a safe environment for the health care to be provided.
How a Home Health Aide/Personal Care Aide Support a Patient’s Rights
(adapted from Leahy, Fuzy & Grafe, 2013)
- Never abuse a patient in any way. Complete all tasks and provide excellent care for patients. Never neglect their care.
- Report any suspected instance of abuse or neglect to a supervisor immediately.
- Keep all patient information confidential. Never discuss patient information in a public place.
- Do not gossip about a patient to friends or family. Never discuss patient information with people outside of the health care team.
- Never leave patient records unattended. If using a computer, use a protected password. Close the browser and log out of a patient’s record before walking away from the computer.
- Don’t leave messages with identifying patient information on voice mail messages or with people who are taking messages.
- Don’t put patient identifying information in emails. Do not keep patient information on a personal computer or other personal electronic devices.
- Shred documents as the agency directs. Never throw documents with patient identifying information out in the regular garbage.
- Do not take pictures while at a patient’s home. Do not take pictures of a patient with a personal camera. Do not take photos of a patient’s home or belongings.
- Do not share information about a patient or their family on social networking sites. Never discuss patient names, addresses, or information with which others could identify the patient.
- Never tell or bring a family member or friend to a patient’s home during or in between work hours.
- Always knock on a patient’s door before entering the house or a room they are in.
- Never open or read a patient’s mail.
- Call the patient by their preferred name. Don’t use baby talk with adults.
- Involve the patient in the planning of their care and let them make choices and complete any task independently that they can.
- Never automatically touch a patient or complete a task without seeking permission first.
- If a patient refuses a service or treatment, respect their right to do so. Document and report the refusal.
- Do not accept gifts or money from a patient or their family.
- If you shop for groceries or other items for a patient, use the money as directed.
- Document all care provided carefully, timely, and truthfully. Be accurate with the amount of time provided care. Never document care that was not provided.
Advanced Directives
Advanced Directives are legal documents that allow a person to choose the type of medical care they wish to receive should they become unable to state their choices and make decisions in the future (Leahy, Fuzy & Grafe, 2013)
An advanced directive is a legal document that tells a healthcare provider the type of treatments a patient wishes and does not wish to receive. They also allow a patient to select an individual(s) to make decisions for them should they be unable to do so. There are many types of advanced directives, which can be further explored by visiting MedlinePlus at http://www.nlm.nih.gov/medlineplus/advancedirectives.html
Living Wills
Living wills are a type of an advanced directive. They explain the type of medical care a patient wants and does not want to receive should they be unable in the future to make decisions for themselves.
A living will is not the same as a last will and testament. A last will and testament is a legal document that delegates a person to be an executor of their estate and explains how a person wishes to have their property and possessions disposed of after their death. A living will is only about medical care and treatment.
Laws about living wills vary from state to state. Examples of what a person may include in their living will might be decisions about:
- Being artificially fed through a vein or stomach
- Having a tube inserted down their throat for mechanical ventilation
- CPR
- Blood transfusions
- Dialysis
Durable Power of Attorney for Health Care (a.k.a. Health Care Proxy)
A health care proxy is someone who the patient designates to make decisions for them in the future should they be unable to do so. A health care proxy is a type of advanced directive. A health care proxy is not the same as an executor of a will. A patient can have one person as the executor of their will and a completely different person designated as their health care proxy if they choose. A health care proxy can make decisions for a patient’s health care if the patient is unable to do so. A health care proxy is responsible for carrying out a patient’s wishes and for following a living will. If the patient has not made a living will, the health care proxy is responsible for making decisions on behalf of the patient according to what they believe is in the best interests of the patient.
Laws about health care proxies and the decisions they can make vary from state to state (Health care agents, 2014). Most states do not allow a doctor or other health care provider to be a patient’s health care proxy. Home Health Aides/Personal Care Aides should not agree to be their patient’s health care proxy. This would be a boundary violation.
Do-Not-Resuscitate (DNR) Order
A Do–not–resuscitate (DNR) is another type of advanced directive. A patient who has a DNR has made a decision to not receive CPR (cardiopulmonary resuscitation). This means that should the patient’s heart stop, or if the patient stops breathing, that the health care providers are not allowed to perform CPR. A DNR order is an order that is written by a physician after the patient has discussed their wishes with their doctor (Do-not-resuscitate order, 2014). If a patient has a DNR order and a health care provider performs CPR knowing there is a DNR order, legal consequences can occur against the health care provider. It is important to know whether your patient has a DNR order in place.
Having a DNR order does not affect any other treatments the patient receives. This means that a patient can continue to receive treatments such as medications, surgeries, physical therapy, and all other medical interventions. A DNR order only applies to whether or not your patient would like CPR performed should their heart stop or if they stop breathing.
A health care proxy or family member cannot have a DNR order removed if it was already in place, based on the patient’s wishes and discussion with their doctor. This means that even a patient’s health care proxy cannot revoke (have removed) a DNR order if the patient had one in place before they became unable to make their own choices.
Self-Check M2-16
Decide whether the statement is True or False
- Patients have a right to considerate and respectful care. _______
- Patients have a right to review their medical records and to control who can access their records and medical information. _______
- You can share medical information about your patient with any family member who wants to know how the patient is doing. ______
- Patients have a right to refuse medical treatment even if you think they should have the treatment. ______
- The patient has a responsibility to inform their healthcare team about who their health care proxy is and if there are any changes in their medical condition._______
- A patient who has a DNR order can still continue to receive home health services, medications, and treatments. _______
- A DNR order is a physician order based on the patient’s wishes, which states should the patient stop breathing, or their heart stop beating, CPR will not be performed.________
- If a patient has a DNR order, the patient’s family can get it removed. _________
- A health care proxy is someone the patient selects who can make decisions for the patient should the patient become unable to do so. _______
- A health care proxy can have a DNR order removed because they know what is best for the patient. ________
Confidentiality
Confidentiality means keeping what is supposed to be private, private. It means not disclosing (telling) other people who do not have a right to know information about the patient. Protecting a patient’s confidentiality means not sharing information with others (outside of the health care team) who the patient does not want to know the information. Home Health Aides/Personal Care Aides will come to know intimate details about their patient’s body and lives. They must take every step that they can to protect this privileged information. They have an ethical and a legal responsibility for protecting the privacy of their patient. A good rule of thumb to use before sharing patient information with members outside of the healthcare team is to ask :
- Does this person have a right to know this information?
- Did the patient give me permission to share information with this person?
- Would sharing this information be harmful to the patient?
- Would I want someone to know this information if it were me?”
Health Insurance Portability and Accountability Act (HIPAA)
In 1996, the Health Insurance Portability and Accountability Act (HIPAA) was passed by Congress. This law is designed to protect people’s privacy with regard to their health and health care. This law gives people rights over the medical information, including the right to receive a copy of their medical records, the right to correct incorrect information in their medical record, and the right to control who has access to their records. You can read more about privacy rights of HIPAA at the U.S. Department of Health and Human Services website: http://www.hhs.gov/ocr/privacy/hipaa/understanding/
Legal Ramifications for HIPAA Violations
If health care workers violate a patient’s privacy, they and/or their agency or the organization for which they work can be fined or imprisoned. The American Recovery and Reinvestment Act of 2009 established a penalty structure for HIPAA violations. Civil and criminal penalties can result if an individual health care worker and/or a health care agency does not comply with HIPAA.
According to the American Medical Association (n.d), fines can range from $100 per incident in a case where the worker was not aware of making a violation to $50,000 for violations which are willful (on purpose) and are not corrected within a specified time frame. Imprisonment sentences can range from one year to up to ten years. You can read more about specific fines for violations of HIPAA at: http://www.ama–assn.org/ama/pub/physician–resources/solutions–managing–your–practice/coding–billing–insurance/hipaahealth–insurance–portability–accountability–act/hipaa–violations–enforcement.page
Self-Check Activity M2-17
Identify which of these scenarios is a HIPAA violation by indicating yes or no.
- Telling your best friend to meet you at your patient’s house to go to lunch. ______
- Telling your supervisor that your patient has a wound on their buttocks. ______
- Calling the nurse while you are at your patient’s house to let her know the patient has run out of medications. ______
- Telling your fellow co-worker details about your patient’s health care while you are at the movies. _______
- Telling your patient’s son details about your patient’s health care after your patient told you not to. ______
Post-test
M2-PT
- Put in order of importance, or the order in which needs should be met, the following needs from Maslow’s Hierarchy of Needs:
- Safety and Security Needs
- Love and Belonging Needs
- Physical Needs
- Self-actualization Needs
- Self-esteem Needs
- Which of the following statements best reflects cultural competence?
- Telling an Asian child, “You must get all A’s in math because all Asians are good at math.”
- Telling a Spanish speaking patient, “You are in America now. You should learn to speak English.”
- Telling your boss, “I will only work with Caucasian patients.”
- Asking your patient who is Native American, “Tell me about your beliefs so that I can understand you more.”
- True or False: It is important to find out your patient’s gender preference, preferred name, and who is considered to be part of their family to ensure health care is provided in a culturally competent manner.
- Which of the following is NOT a cliche?
- “It will all work out for the best.”
- “I know exactly how you feel.”
- “Hang in there. It will get better.”
- “You sound as if you are feeling scared. Would you like to talk about it?”
- “We are never given more than we can handle.”
- Which of the following are nonverbal methods of communication? Select all that apply.
- Nodding
- Tone of voice
- Crossing arms over the chest
- Eye contact
- Touching a shoulder
- How near a person stands to another
- Slouching in a seat
- Rolling of the eyes
- Sighing
- Which of the following are things you can do to show you are a good listener? Select all that apply.
- Face the person you are speaking.
- Respect cultural differences and beliefs
- Avoid calling patients “honey” or “dear” and use their preferred name of address.
- Provide silence so a patient can gather their thoughts.
- Restate what you heard the patient say and ask for clarification when you are unsure of what they are trying to express.
- Don’t finish the patient’s sentences or interrupt them while they are speaking.
- Which of the following is an effective means of communicating with a person who has a hearing impairment?
- Shout as loud as you can.
- Stand behind the patient while talking to them.
- Use a high pitched and loud voice.
- Avoid talking to the patient at all, because they can’t hear you anyway.
- Stand in front of the patient and use a clear, low voice while speaking.
- Which of the following is an effective way to help a person with a visual impairment?
- Ensure the patient wears their glasses.
- Use the clock method to indicate where food is during mealtimes.
- Ensure the patient knows the objects in their path while walking.
- Keep the environment clutter free to avoid falls.
- Read aloud to the patient if they are unable to do so.
- What is the best way to establish a therapeutic relationship?
- Don’t allow patients to make choices. Tell them what to do.
- Arrive to work on time and complete assigned tasks.
- Do things for the patient they are able to do independently, as it is important they rely on the home care worker as much as possible.
- Tell anyone who asks about the patient as much information as you know.
- True or False: It is okay to continue to visit a patient once they are no longer receiving home care services from the agency.
- Which of the following is an example of objective information that can be included in documentation?
- “The patient was very rude to me this morning when I tried to bathe him.”
- “The patient’s right leg is swollen, red, and warm to the touch.”
- “I don’t think the patient should be allowed to visit with their family because she cries when they leave.”
- “I think the patient has a cold because he sneezed a lot today.”
- True or False: Documentation should be completed immediately after a home care visit once tasks have been completed, and before moving on to work with the next patient.
- True or False: An error in documentation should have one line drawn through it with the home care worker’s initials and the date next to the error.
- True or False: It is okay to document all the tasks on the home care worker’s assigned task list before they are completed.
- True or False: Abuse that is witnessed or suspected must always be documented and reported to a supervisor immediately.
- Which of the following are examples of abuse and/or neglect? Select all that apply.
- Bite marks
- Yelling at a patient
- Violence witnessed in the home
- Not pureeing food as directed in the Care Plan, for a patient who cannot chew
- Harshly pushing a fork into a patient’s mouth when they refuse to open their mouth
- Allowing a patient to lie in their own urine or feces
- Burn marks
- Pressure ulcers
- True or False: Patients have a right to be informed of the health care they are to receive and they have a right to refuse treatment and make decisions about their own health care.
- Which of the following are ways to protect patient confidentiality? Select all that apply.
- Only share information with people the patient designates can receive information.
- Don’t include identifying patient information in voicemails or emails.
- Don’t take photos of a patient, their home, or belongings.
- Don’t talk about patients in public places.
- Don’t tell family, friends, or people outside the healthcare team information about the patient.
- True or False: A DNR order is a physician order which states the patient does not want CPR to be performed.
- True or False: HIPPA is a law that protects a patient’s right to privacy about their health care. If a HHA/PCA violates this right to privacy, it can result in monetary fines, prison sentence, and/or getting fired.
1). C
2). A
3). E
4). B
5). D
Feedback:
1. Allowing a patient time to pray before they eat helps a patient meet their Love/Belonging Needs. As humans, we all have a need to belong to a community and to feel connected to people and things outside of ourselves. Praying allows a patient to maintain a connection with their religious beliefs and community.
2. Assisting a patient with eating and dressing helps to meet basic physical needs of obtaining food and protecting their bodies with clothing. Helping patients complete ADLs is an important task of the HHA/PCA.
3. A HHA/PCA can assist a patient meet their goals by encouraging independence. Goals will vary by patient and change throughout our lives. They can be affected by illness and disability. Goals we set for ourselves can help us be the best we can be. This helps to ensure Self-actualization Needs.
4. Meeting a patient’s Safety/Security Needs is an important task of the HHA/PCA. Teaching a patient how to use ambulation devices (e.g. walkers and canes) helps to ensure their safety and reduce the risk of injury to the patient.
5. Providing praise and encouragement for completion of any task, no matter how small allows the HHA/PCA to help patients meet their Self-esteem Needs.
1). B
2). A
3). D
4). C
5). F
6). E
Feedback:
1. A stereotype is the belief that all members of a group are the same. We often develop stereotypes from our family and the media. Believing that men should not cry is a stereotype.
2. Ethnocentricism is the belief that our own culture is better or superior to other cultures. The statement, “Everyone who comes to the United States should learn to speak English” suggests that living in the United States and speaking English is better than living in other countries or speaking other languages.
3. Race is a classification of people based on physical attributes, geographic ancestry (where a person came from originally), and inherited characteristics. Identifying as Native American is a type of race.
4. Culture is a set of behaviors, beliefs, values, attitudes, and goals shared by a group of people. A person may identify themselves as belonging to many cultures. Identifying as Italian indicates belonging to a specific cultural group.
5. Diversity means including and respecting different types of cultures. An agency who hires people of all genders, races, religions, and cultures demonstrates that they value differences.
6. Racism is a belief that one racial group is better than another racial group, or that one member of a race is the same as all other members of that race. If an agency only hires members of one particular race they are discriminating against others races. Racism results in prejudice against a particular race.
a. Cultural competence
b. Cultural awareness
Feedback:
1. Cultural competence means the ability to incorporate cultural awareness into the health care practice. Doing so demonstrates understanding, honor, and respect for a patient’s cultural beliefs.
2. Cultural awareness means how aware you are about the values and beliefs of other cultures and how much you appreciate the various aspects of the different cultures.
1. True
2. False
Feedback:
1. Many African Americans do have a strong sense of family and spiritual faith.
2. There are many terms that people may use to identify themselves. Remember, a shared complexion does not necessarily mean there is a shared culture. It is important to find out the terms a patient uses to define their identity.
1. True
2. True
Feedback:
1. Many Asian people typically take the context of the situation in mind. This means that they pay careful attention to nonverbal cues during conversation such as gestures, tone of voice, eye contact, and silence. It is important to remember to pay attention to the nonverbal cues you are using as well as those being used by your patient in order to have the best understanding of the meaning behind what is being conveyed.
2. Generally, Asians tend to be group and family oriented which is known as belonging to a collectivist culture. Therefore, decisions and actions are made as part of a group and with consideration to the effects on the group. Honor and respect should be shown to the entire family.
1. True
2. True
Feedback:
1.Latinos often have a very deep sense of family connection, called familismo. Family may include extended members of the family and close friends whom they trust.
2. Due to the strong sense of family, it is to include all members of the family during health care decision making and care provision. This will help the patient and family to trust and be willing to work with the health care worker.
1. True
2. False
Feedback:
1. People of the Middle East may often prefer to have same-sex caregivers. Direct eye contact with members of the opposite sex is often frowned upon. Health care workers should check with the family to determine gender preferences for caregivers.
2. People from the Middle East traditionally have a strong sense of affiliation with their family. Families and friends may be very close-knit and involved in the healthcare of the patient, with the elder member of the family expecting to be involved in health care decisions
1. B
2. B
Feedback:
1. Verbal communication involves the use of words or sounds, which are either spoken or written. Nonverbal communication is the way we communicate without using words. It can include: shaking a head, rolling eyes, smiling, tone of voice, body language, or crying. Saying, “I don’t care” is a method of verbal communication. Shrugging shoulders is a nonverbal method of communication.
2. Calling a dog to come is a method of verbal communication as spoken words are used. Clapping one’s hands to get the attention of a dog or person is a method of nonverbal communication.
1. True
2. False
3. False
4. True
5. True
Feedback:
1. It is important to ensure a person with a visual or hearing impairment can communicate with others as well as possible. Ensure patients who need them have glasses on and hearing aids in to best help them communicate with others.
2. Telling a patient not to worry and that “Things will get better” are uses of clichés. Clichés are catch phrases people use repeatedly that do not really mean anything at all. They discount what another person is feeling and discourage them from fully expressing their feelings and thoughts.
3. Closed-ended questions such as “yes/no” and asking many “why?” questions are ways to end conversation and discourage a patient from fully expressing their feelings and thoughts. Instead, use open-ended questions such as, “Tell me about your pain.”
4. Providing alternative forms of communication such as a chalkboard or paper and pen may help a person who has difficulty speaking communicate their needs to others.
5. People with a speech or cognitive disorder may be especially aware of body language being used by people with whom they are communicating. It is important to be aware of nonverbal messages such as tone of voice and posture that you send during communication.
Scenario 2 demonstrates active listening.
Feedback:
The healthcare worker stopped completion of her tasks, positioned herself so she could focus on her patient and so that her patient would know she cared about what she had to say. She also used reflection and an open-ended question, inviting Mrs. Williams to share her thoughts and feelings.
1. No
2. Yes
3. Yes
4. Yes
5. No
6. Yes
7. No
8. No
9. Yes
10. Yes
Feedback:
1. Following directions as stated in the care plan is providing competent care. This would not be a boundary violation.
2. Staying past the time your agency/supervisor has established is considered to be a boundary violation. This can indicate possessiveness of the patient and can lead to a breakdown in the care of the patient among members of the healthcare team.
3. Taking money or gifts from a patient or their family is considered to be a boundary violation and is unprofessional behavior. Many agencies have policies prohibiting this type of behavior.
4. Continuing to visit a patient once the relationship has ended is considered to be a boundary violation. While ending a relationship can stir up various emotions, it is wise for the HHA/PCA to discuss these emotions with their supervisor rather than with the patient. Many companies have specific policies about termination of relationships.
5. Providing a bed bath as required by the care plan is an assigned task and is considered to be providing competent care, which is not a boundary violation.
6. Visiting a patient outside of working hours is considered to be a boundary violation and is unprofessional behavior. This can indicate possessiveness of the patient and can lead to a breakdown in the care of the patient among members of the healthcare team. Many agencies may have policies in place to prohibit this type of behavior.
7. Turning and positioning a patient in bed is performing competent care and is not a boundary violation.
8. Informing a supervisor about suspicions of abuse is an important aspect of a HHA/PCA’s responsibilities and is not considered a boundary violation.
9. Using a patient’s food for your personal use is a boundary violation and should never be done. Many agencies may have policies in place to prohibit this type of behavior.
10. Keeping a secret from the rest of the health care team is a boundary violation. It is important to always inform your supervisor about important statements patients make about their health care, especially statements indicating suicidal thoughts or abuse.
1. Subjective
2. Objective
Feedback:
1. A patient’s report of symptoms is subjective information as it is something the health care worker did not or cannot observe.
2. Directly observing an increase in swelling of a patient’s leg is objective information as it can be measured.
1. 1300
2. 1800
3. 2330
4. 0330
5. 1200
6. 10:00 pm
7. 7:30 pm
8. 6:15 pm
9. 11:30 pm
10. 1:00 pm
Feedback:
1. 1 pm= 1 +12=13.The time is 1300 hours on a 24-hour clock.
2. 6pm= 6 + 12= 18. The time is 1800 hours on a 24-hour clock.
3. 11:30 pm= 11.30 + 12= 12.30. The time is 2330 on a 24-hour clock.
4. 3:30 am= 0330 on a 24-hour clock.
5. 12:00 am = 1200 on a 24-hour clock.
6. 2200= 22-12= 10:00 pm
7. 1930= 19-12=7. Add the 30= 7:30 pm
8. 1815= 18-12=6. Add the 15= 6:15 pm
9. 11:30= 23-12= 11. Add the 30= 11:30 pm
10. 1300= 13-12=1. The time on a 12-hour clock is 1:00 pm
1. False
2. True
3. False
4. True
5. True
Feedback:
1. Never use white out to fix an error. Patient charts are legal records. Draw a single line through it and put initials and date next to the error. Then, write in the correct information.
2. When documentation is complete, Home Health Aides/Personal Care Aides should sign it with their full name and title.
3. Documenting care prior to performing it is considered to be falsifying records.
4. Due to the difficulty in keeping track of observations made, care should always be documented immediately after performing it.
5. Judgmental statements or personal opinion should never be included in the patient care record. Objective observations, those that can be observed or measured and subjective information, symptoms the patient reports are types of information that should be included within the HHA/PCA’s documentation.
ALL ANSWERS ARE SIGNS OF ABUSE
Feedback:
Bite marks, unexplained bruises, observing or learning about a family member or friend stealing jewelry or money from a patient, yelling, name-calling, or using threats are all signs of abuse. Not properly cleaning a patient or turning and positioning a patient every two hours are considered to be neglect and are also forms of abuse.
1. True
2. True
3. False
4. True
5. True
6. True
7. True
8. False
9. True
10. False
Feedback:
1. According to the Patient Bill of Rights, patients have a right to considerate and respectful care.
2. According to the Patient Bill of Rights, patients have a right to request and receive a copy of their medical record. This is also a federal law under HIPAA guidelines.
3. You cannot share any information about the patient without the patient’s specific consent.
4. According to the Patient Bill of Rights, patients have a right to refuse treatment.
5. According to the American Hospital Association, 1992, Patient Responsibilities include informing their healthcare team about who their health care proxy is and if there are any changes in their medical condition.
6. A patient who has a DNR order can still continue to receive home health services, medications, and treatments. A DNR order will only prohibit CPR and artificial respiration to occur should the patient choose to obtain this physician order.
7. A DNR order is a physician order based on the patient’s wishes, which states should the patient stop breathing, or their heart stop beating, CPR will not be performed.
8. It is a patient decision about whether or not to have a DNR order. If the patient is conscious and oriented, the family cannot have a DNR order removed.
9. A health care proxy is someone the patient selects who can make decisions for the patient should the patient become unable to do so.
10. If the patient is conscious and oriented, it is a patient decision and not up to the family about whether or not to have a DNR order.
1. Yes
2. No
3. No
4. Yes
5. Yes
Feedback:
1. It is a HIPAA violation to tell your family and friends about a patient. Having them meet you at a patient’s house violates the patient’s privacy.
2. It is not a HIPAA violation to inform your supervisor about your patient’s condition. Any person who is part of the patient’s treatment team is allowed to have information about the patient in order to provide the best care.
3. It is not a HIPAA violation to call the nurse from your patient’s home as the nurse is part of the treatment team and is allowed access to patient information.
4. It is a HIPAA violation to talk about a patient with your co-workers in a public place. Other people who are not involved in the patient’s care can easily overhear your conversation. This would be a violation of the patient’s privacy.
5. It is a HIPAA violation to inform anyone about the details of your patient or their care, unless the patient has given you consent to do so. This includes family members. If a patient does not want a family member to know the details of their care, that is their choice and you must uphold their confidence and privacy.
1. C, A, B, E, D
2. D
3. True
4. D
5. These are all nonverbal methods of communication
6. All are ways to show you are a good listener
7. E
8. All are effective ways to help a person with a visual impairment
9. B
10. False
11. B
12. True
13. True
14. False
15. True
16. All are signs of abuse or neglect
17. True
18. All are ways to protect patient confidentiality.
19. True
20. True
References
Advance directives. (2014, May 5). Retrieved from http://www.nlm.nih.gov/medlineplus/advancedirectives.html
American Academy of Pediatrics. (2015, May 5). Different types of families: A portrait gallery. Retrieved from https://www.healthychildren.org/English/family-life/family-dynamics/types-of-families/Pages/Different-Types-of-Familes-A-Portrait-Gallery.aspx
American Atheists. (n.d.). What is atheism? Retrieved from http://atheists.org/activism/resources/what–is-atheism
American Hospital Association. (1992). A patient’s bill of rights. Retrieved from http://www.qcc.cuny.edu/SocialSciences/ppecorino/MEDICAL_ETHICS_TEXT/Chapter_6_Patient_Rights/Readings_The%20Patient_Bill_of_Rights.htm
American Medical Association. (n.d.). HIPAA violations and enforcement. Retrieved from http://www.ama–assn.org/ama/pub/physician–resources/solutions–managing–your–practice/coding-billing-insurance/hipaahealth-insurance-portability-accountability-act/hipaa-violations-enforcement.page
BBC. (2009, June 12). Judaism at a glance. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/ataglance/glance.shtml
BBC. (2009, June 30). Islam at a glance. Retrieved from http://www.bbc.co.uk/religion/religions/islam/ataglance/glance.shtml
BBC. (2009, July 9). Hanukkah. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/holydays/hanukkah.shtml
BBC. (2009, July 15). Sabbath. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/holydays/sabbath.shtml
BBC. (2009, August 13). The Torah. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/texts/torah.shtml
BBC. (2009, August 14). The basics of Christian beliefs. Retrieved from http://www.bbc.co.uk/religion/religions/christianity/beliefs/basics_1.shtml
BBC (2009, August 18). Mosque. Retrieved from http://www.bbc.co.uk/religion/religions/islam/prayer/mosque.shtml
BBC. (2009, September 3). Hijab. Retrieved from http://www.bbc.co.uk/religion/religions/islam/beliefs/hijab_1.shtml
BBC. (2009, September 8). Five pillars of Islam. Retrieved from http://www.bbc.co.uk/religion/religions/islam/practices/fivepillars.shtml
BBC. (2011, June 30). Christianity at a glance. Retrieved from http://www.bbc.co.uk/religion/religions/christianity/ataglance/glance.shtml
BBC. (2011, July 5). Ramadan. Retrieved from http://www.bbc.co.uk/religion/religions/islam/practices/ramadan_1.shtml#practices
BBC. (2011, July 14). Qur’an. Retrieved from http://www.bbc.co.uk/religion/religions/islam/texts/quran_1.shtml
BBC. (2011, July 19). Basic articles of faith. Retrieved from http://www.bbc.co.uk/religion/religions/islam/beliefs/beliefs.shtml
BBC. (2011, September 1). Eid al-Fitr. Retrieved from http://www.bbc.co.uk/religion/religions/islam/holydays/eidulfitr.shtml
BBC. (2011, September 23). Rosh Hashanah. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/holydays/roshhashanah.shtml
BBC. (2011, October 6). Yom Kippur: The Day of Atonement. Retrieved from http://www.bbc.co.uk/religion/religions/judaism/holydays/yomkippur.shtml
Carteret, M. (2010, October 21). Cultural values of Asian patients and families. Retrieved from http://www.dimensionsofculture.com/2010/10/cultural-values-of-asian-patients-and-families/
Carteret, M. (2010, October 21). Folk illnesses and remedies in Latino communities. Retrieved from http://www.dimensionsofculture.com/2010/10/folk–illnesses–and–remedies–in–latino–communities/
Carteret, M. (2010, October 21). Healthcare for Middle Eastern patients and families. Retrieved from http://www.dimensionsofculture.com/2010/10/health-care-for-middle-eastern-patients-families/
Carteret, M. (2010, October 21). Traditional Asian health beliefs and healing practices. Retrieved from http://www.dimensionsofculture.com/2010/10/traditional-asian-health-beliefs-healing-practices/
Carteret, M. (2010, November 3). Cultural aspects of death and dying. http://www.dimensionsofculture.com/2010/11/cultural-aspects-of-death-and-dying/
Carteret, M. (2010, November 3). The importance of familismo. Retrieved from http://www.dimensionsofculture.com/2010/11/the-importance-of-familismo/
Carteret, M. (2011, March 15). Cultural values of Latino patients and families. Retrieved from http://www.dimensionsofculture.com/2011/03/cultural-values-of-latino-patients-and-families/
Carteret, M. (2011, May 16). Healthcare for African American patients/families. Retrieved from http://www.dimensionsofculture.com/2011/05/health–care–for–african–american–patientsfamilies/
Do-not-resuscitate order. (2014, May 7). In A.D.A.M. Medical Encyclopedia. Retrieved fro http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000473.htm
Gorski, P. C. (1995). Circles of my multicultural self. Retrieved from http://www.edchange.org/multicultural/activities/circlesofself.html
Health care agents. (2014, May 11). In A.D.A.M. Medical Encyclopedia. Retrieved from http://www.nlm.nih.gov/medlineplus/ency/patientinstructions/000469.htm
Kauai’s Hindu Monastery. (n.d.). Basics of Hinduism. Retrieved from https://www.himalayanacademy.com/readlearn/basics/nine-beliefs
Leahy, W., Fuzy, J., & Grafe, J. (2013). Providing home care: A textbook for home health aides (4th ed.). Albuquerque, NM: Hartman.
National Council of State Boards of Nursing. (2014). A nurse’s guide to professional boundaries. Retrieved from https://www.ncsbn.org/ProfessionalBoundaries_Complete.pdf
PBS. (1999). Thailand on television: Basics of Buddhism. Retrieved from http://www.pbs.org/edens/thailand/buddhism.htm


